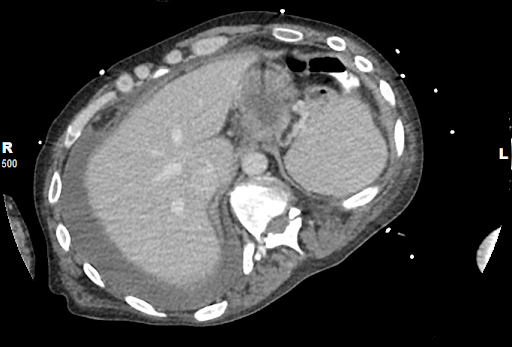
Case Presentation: A 45-years-old African American male with a past medical history of seizure disorder, chronic alcohol abuse, and cervical spine injury, presented to hospital after a witnessed tonic-clonic seizure episode that resolved spontaneously. Initial evaluation revealed hypotension (90/57mmHg), tachycardia (145), tachypnea (36), temperature of 39.1 degrees celsius, leukocytosis (24.2×10^3/microliter) with bandemia, and lactate of 5.7mmol/L. Seizure was presumed secondary to alcohol withdrawal, and patient was admitted to Intensive Care Unit for further management of septic shock. Patient also developed worsening dyspnea, desaturating to 84% on room air. Patient reported chronic diarrhea (with lipase elevated at 149 U/L) likely secondary to pancreatic insufficiency, for which he was started on creon with meals. Computed Tomography (CT) of chest and abdomen showed pancreatic duct dilatation with pancreaticopleural fistula (PPF) extending from the pancreatic duct, through the left upper abdominal quadrant (containing several gas foci) to left lower lobe of the lung. Left pleural space with a thick walled cavitation. Thoracocentesis attempted, however no fluid was obtained. Endoscopic retrograde cholangiopancreatography (ERCP) confirmed a dilated pancreatic duct with leak in the distal tail, and a pancreatic stent was placed to allow drainage into the duodenum. Blood cultures at this time resulted positive for Klebsiella pneumonia, with negative urine studies, source attributed to the PPF. Patient initially received empiric antibiotics (intravenous vancomycin and zosyn) which was deescalated to intravenous ceftriaxone according to culture and sensitivities. Patient clinically improved with shock resolved, and was discharged on oral ciprofloxacin with follow-up in two weeks for repeat CT scan.
Discussion: PPF is a rare complication (especially of chronic alcoholic pancreatitis) with an incidence of only 0.4%. It occurs when a posterior pathway forms between the pancreatic duct and the pleura. Most common presentation include dyspnea (65%), abdominal pain (29%), chest pain (23%), and cough (27%). Pleural effusions are also frequently discovered on the left side. Magnetic resonance cholangiopancreatography (MRCP) is the imaging study of choice for diagnosis of these fistulas with a higher sensitivity (80%) compared to CT scan (47%), or even ERCP (78%) as in our patient. There is currently no consensus on the appropriate management of PPF, but it is suggested that first line medical management consists of majorly conservative approach, such as thoracentesis, octreotide, antibiotics, and total parenteral nutrition for 2-3 weeks. If failed, endoscopic treatment with balloon dilation and placement of intraductal stenting can be pursued to restore anatomic continuity can be attempted. Surgery consisting of internal pancreatic drainage and/or pancreatic resections is a last resort.
Conclusions: PPF is a rare complication that may be seen in patients with chronic alcoholic pancreatitis, and requires a high index of clinical suspicion to diagnose, especially in patients with nonspecific symptoms such as dyspnea or chest pain. MRCP being the imaging study of choice for diagnosis.