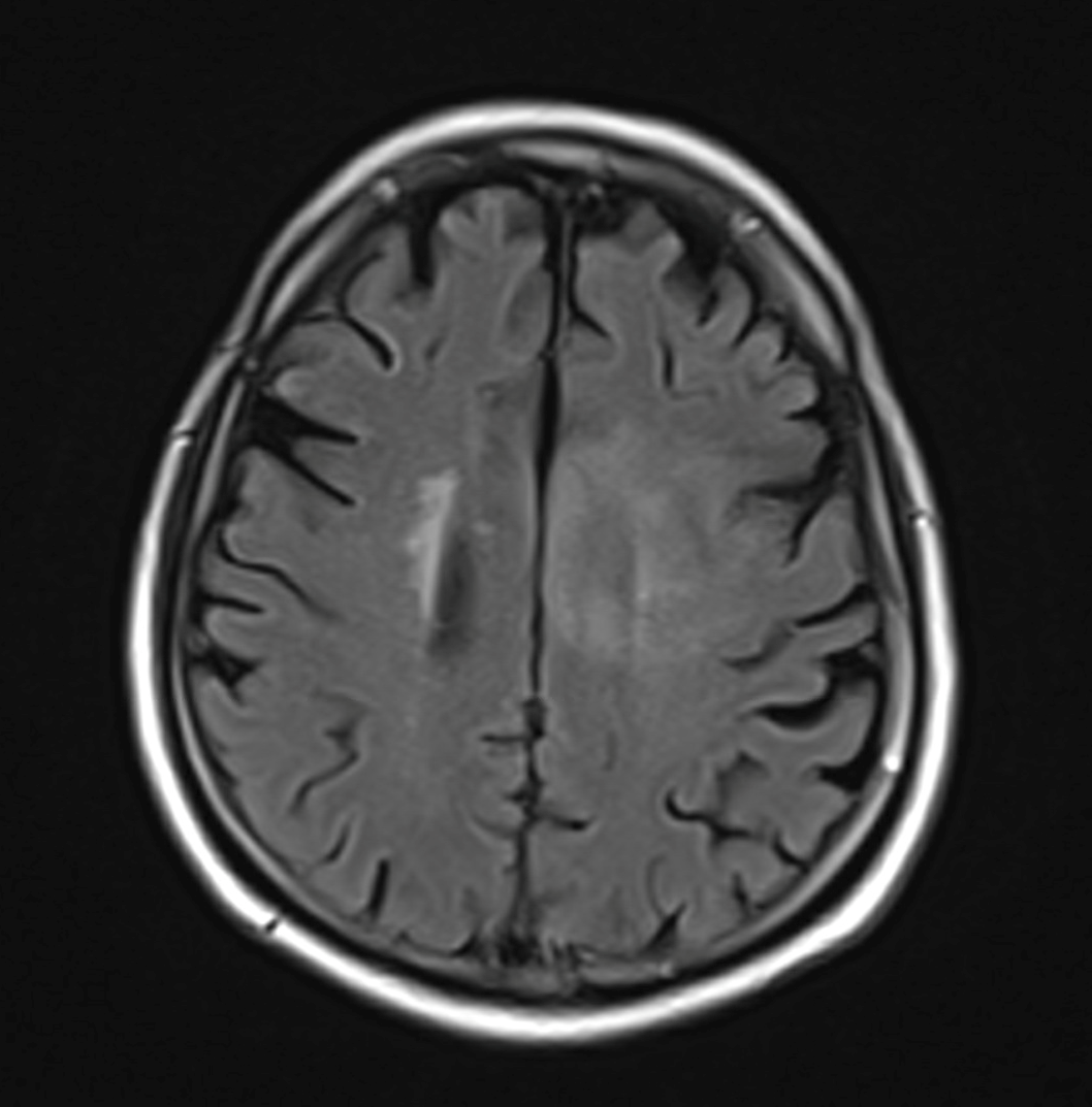
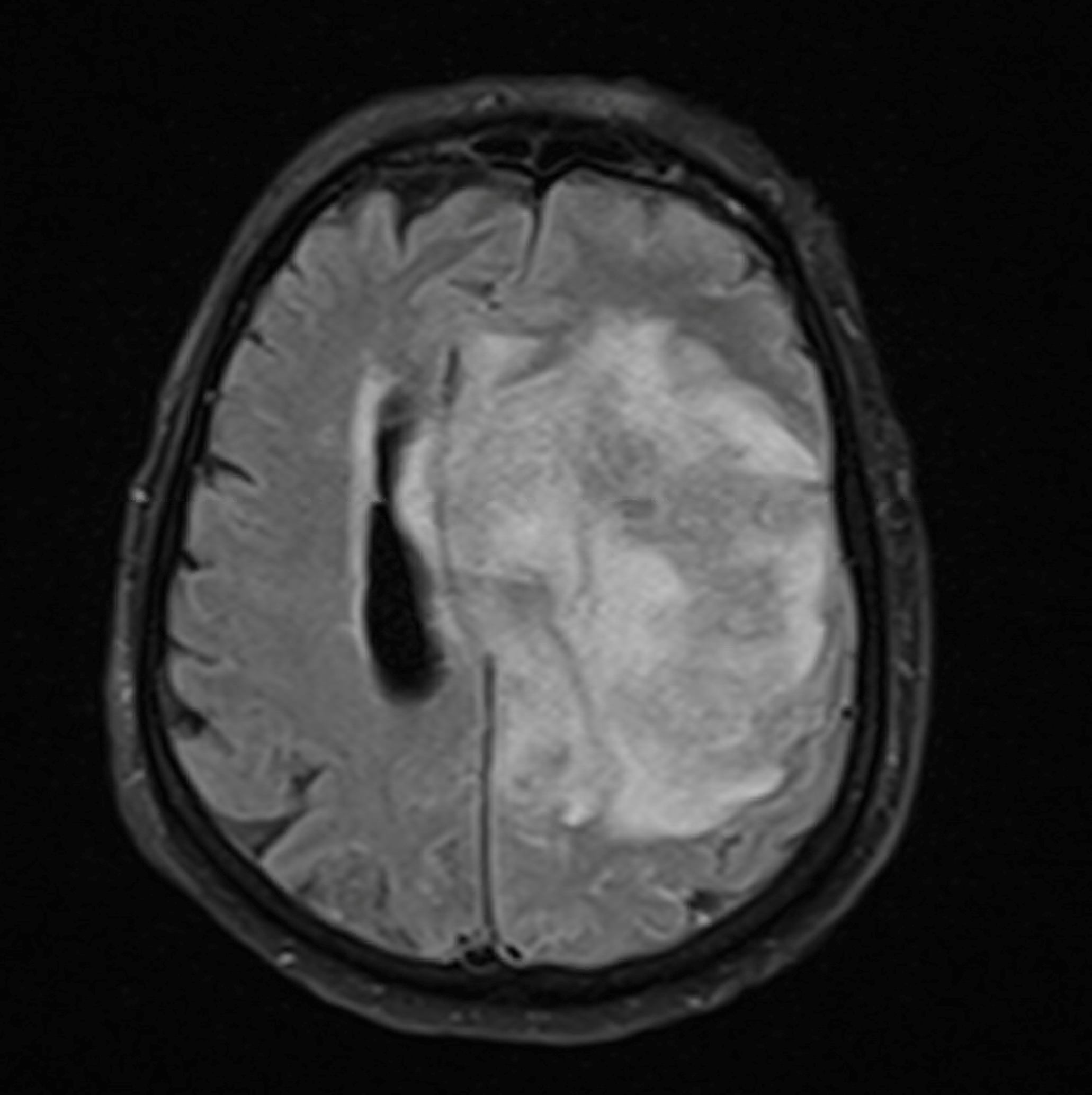
Case Presentation: A 82-year-old male was admitted for generalized weakness lasting several weeks. Past medical history consisted of dilated cardiomyopathy status-post AICD, remote history of large B-cell lymphoma, chronic headache and dizziness for years with worsening over the last several months. Patient’s presentation was notable for low grade fever and hypotension. Physical exam showed a pale, chronically ill-appearing male with global weakness. Remainder of the exam including a neurological evaluation was normal. Routine labs, CT head, echocardiogram, and ICD interrogation were unrevealing. After intravenous hydration, he clinically improved. On day four of hospitalization, he developed acute altered mental status with associated right facial droop, expressive aphasia, fever and leukocytosis. Repeat CT head was negative. Brain MRI showed a left frontal lobe mass suggestive of possible low-grade glioma. The brain lesion was inaccessible for biopsy per Neurosurgical consultation. Patient was started on dexamethasone and antimicrobials to cover for meningitis. The patient deteriorated after lumbar puncture, needing emergent intubation. Repeat MRI showed severe interval progression of large left frontal lobe lesion, significant mass effect and evidence of herniation. Cerebrospinal Fluid (CSF) analysis showed normal glucose, elevated protein and lymphocytic pleocytosis. CSF flow-cytometry and CSF studies for infection were negative. Eventually, the patient declined rapidly and passed away on day nine once his family withdrew care. His brain autopsy showed Acanthamoeba species confirming diagnosis of Granulomatous Amoebic Encephalitis (GAE).
Discussion: Acanthamoeba is a Free Living Amoeba (FLA) found in air, water and soil. It can cause rare but severe infection of skin, eyes and central nervous system. GAE is a life-threatening infection that primarily affects immuno-compromised patients. Its symptoms can include nausea, vomiting, low grade fever and headache to focal motor deficits, seizures, or coma. It is spread by hematogenous route from the skin, sinuses, or lungs, depending on the portal of entry. Timely detection is the key to survival, albeit challenging due to nonspecific and subacute presentation. Clinical features can mimic entities such as neurotuberculosis, neurocysticercosis, viral encephalitis and stroke, leading to delayed diagnosis and high mortality. Diagnostic modalities include CT, MRI, lumbar puncture and biopsy. Biopsy is critical and essential to initiate appropriate medical therapy.Currently, there is no consensus on standard medical management. Survival hinges on combination of timely neurosurgical intervention and initiation of a multitude of antimicrobials such as azoles, anticancer drug miltefosine, pentamidine, and clotrimoxazole.
Conclusions: This case of GAE represents a rare case of encephalitis caused by a ubiquitous FLA. As the population ages and the number of immunosuppressed patients rises, GAE cases will increase. To drive positive outcomes, it will be critical for clinicians to maintain a high index of suspicion and consider GAE in the differential diagnosis of patients with neurological symptoms and brain abscess. In this particular case, the clinical history was investigated post-mortem. However, the potential source or exposure to this organism was not identified.