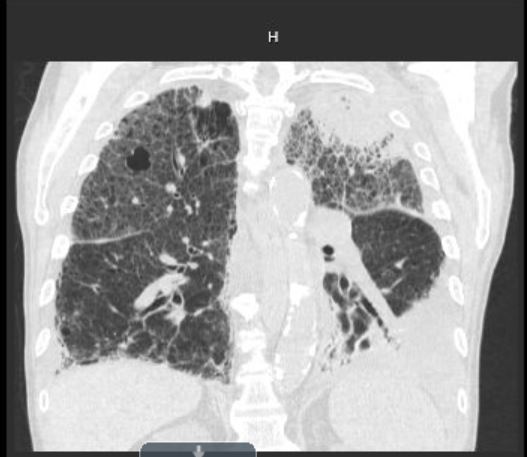
Case Presentation: Case 1: 30 year old woman with uncontrolled T1DM, CKD, recurrent VTE, HTN, recurrent C.Diff, developed leg pain, fever and leukocytosis. Imaging, extensive rheumatology work up and biopsy revealed diabetic myonecrosis, also noted MDRO UTI and C diff colitis treated with ertapenem, ceftriaxone and oral vancomycin. Persistent high grade fever and leukocytosis called for CT chest showing LLL necrotizing pneumonia and pleural effusion. Bronchoscopy revealed large foreign body (3cm x 1 cm) and mucus plugging in her LLL. Cytology revealed non-septate hyphae infiltrating necrotic lung tissue including blood vessels consistent with mycetoma and suppurative inflammation. She was treated with Ambisome and posaconazole alternating isavuconazole due to AKI. After completion of treatment, imaging and symptoms improved.Case 2: 80 year old man with MDS/excessive blasts, CAD and sarcoidosis admitted for fludarabine and Cytarabine. He developed neutropenic fever due to MRSA bacteremia without endocarditis, treated with vancomycin and zosyn along with voriconazole and acyclovir prophylaxis. He had recurring fever, hypoxia and hemoptysis. CT chest revealed mass like lesion >5cm in size. Voriconazole was changed to isavuconazole. BAL showed no lesion in the tracheobronchial region but mucopurulent return with RBC 9000, WBC 134 N 30%, L 14%, H 56%. Despite treatment, he declined and transitioned to comfort care. Limited autopsy of lung tissue showed infiltrated fungal infection with intravascular thrombosis consistent with mucormycosis.Case 3: 23 year old man with stage IVB NSHL on BEACOPP presented with neutropenic fever during RBC transfusion. Infectious work up was negative except worsening rash on LLE. CT leg showed cellulitis. Neutropenia and fever resolved, rash improved with Vancomycin and Zosyn thus was discharged on Bactrim. He returned next day with fever and worsening rash. Sections of the rash were purple, blistering and grey sloughing tissue with golden colored drainage. Skin biopsy of the rash revealed multiple hyphae with ribbon like appearance. MRI leg showed soft tissue cellulitis with fasciitis and periosteal reaction of the lateral tibial diaphysis. He had aggressive debridement by plastic surgery along with Ambisome with transition to posaconazole.
Discussion: Mucormycosis is rare but rapidly progressing infection characterized by infarction and necrosis of the host tissue. It commonly presents as sinusitis caused by inhaled spores. We present different manifestations of the mucormycosis in immunocompromised patients. Initial presentation of the pulmonary and cutaneous mucormycosis can be easily misdiagnosed as pneumonia and cellulitis respectively. High clinical suspicion is important for early diagnosis and initiation of treatment. Cultures often yield no growth. Direct identification of organism on the histopathology reveals the diagnosis. It’s treatment involves surgical debridement when possible, monotherapy with amphotericin B followed by oral posaconazole or isavuconazole. It has a high mortality rate (>85%) specially for pulmonary and disseminated mucormycosis.
Conclusions: Mucormycosis can have various manifestations. As a hospitalist it is important to keep high clinical suspicion of mucormycosis even in absence of sinus infection specially in immunocompromised patients. Diagnosis is made primarily with direct visualization of hyphae.