Background: Interhospital transfer (IHT) is often performed to provide patients with necessary specialized care. While there are numerous examples of racial/ethnic health inequities in our healthcare system, inequities in IHT are not well-characterized. We sought to determine if there are racial/ethnic inequities in IHT among patients with select conditions previously associated with a mortality benefit from transfer.
Methods: We performed a cross-sectional analysis of 2013 Center for Medicare and Medicare Services (CMS) 100% Master Beneficiary Summary and Inpatient claims merged with 2013 American Hospital Association data. Patients with age greater than or equal to 65 and a primary diagnosis of acute myocardial infarction, stroke, sepsis or respiratory disease who were continuously enrolled in Medicare A/B and had an acute care hospitalization claim in 2013 were included; Medicare managed care, ESRD beneficiaries and patients hospitalized at federal, non-acute care or critical access hospitals were excluded. The outcome was transfer, as previously defined by having corresponding “transfer out”/”transfer in” claims from different hospitals or a “transfer out” or “transfer in” claim with corresponding admission or discharge to/from another hospital within 1 day of the claim. The primary predictor was race, as categorized in the CMS dataset (White, Black, Hispanic, Other). We examined patient and hospital characteristics by race, then calculated crude and adjusted odds of transfer by race using univariable then multivariable logistic regression models adjusting for patient age, sex, Medicaid co-insurance, median income for zip-code, diagnosis-related group (DRG) weight, hierarchical conditional category (HCC) comorbidity score, admissions in previous year, season of admission, and accounting for fixed-effects by hospital. Our primary analysis examined odds of transfer among patients with all four diagnoses combined; we also performed secondary analyses stratified by individual diagnoses.
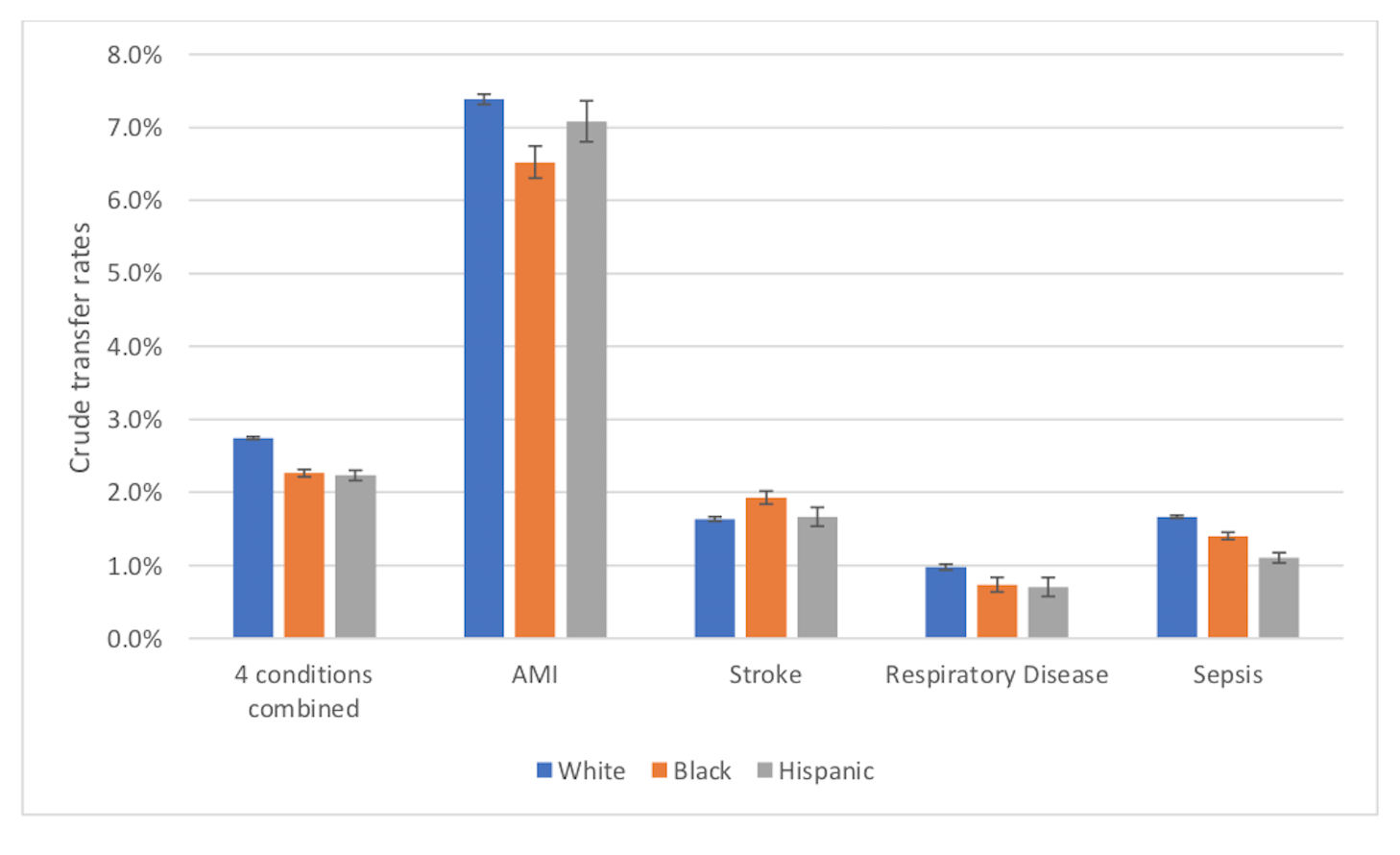
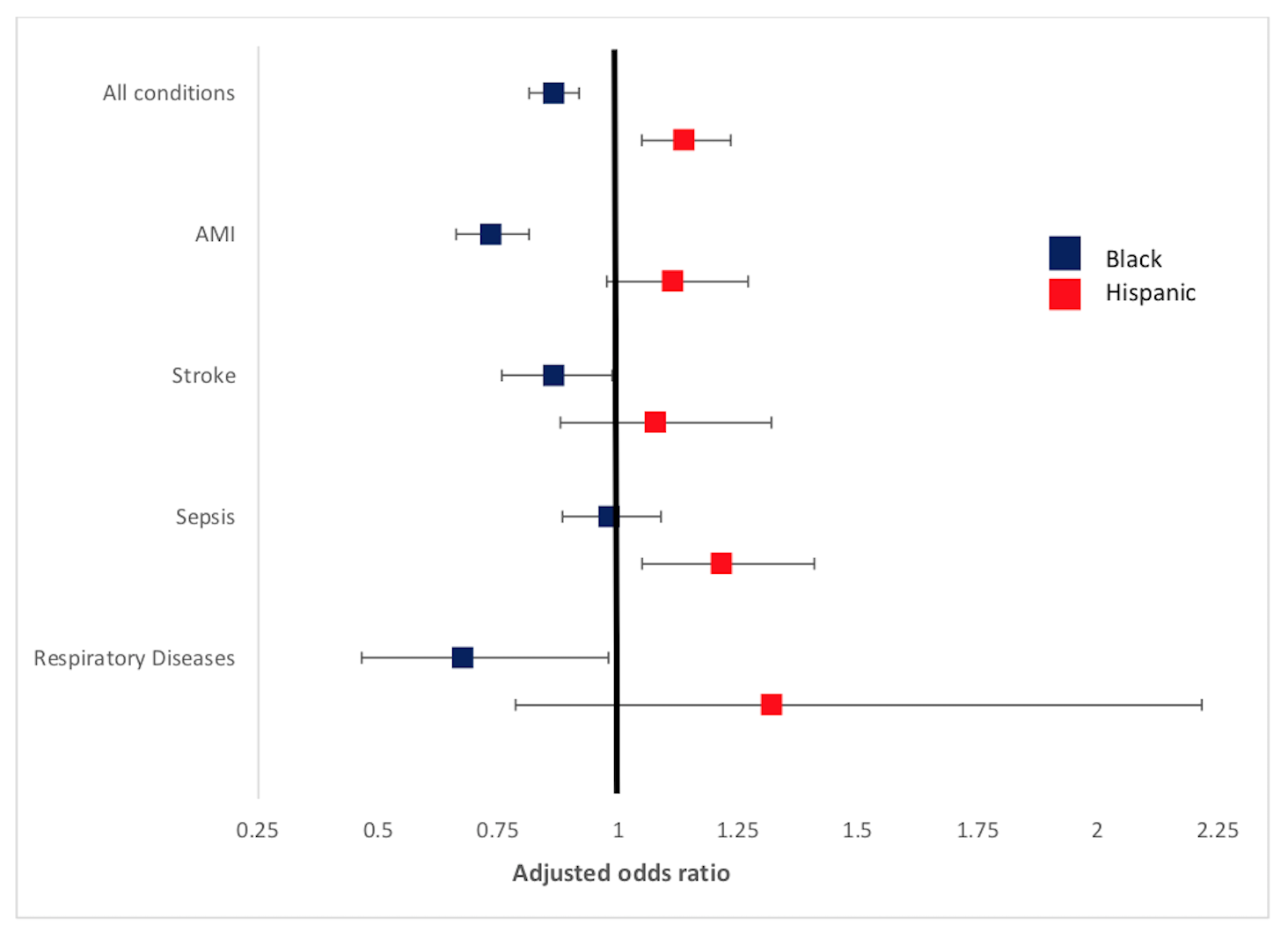
Results: Of the 899,557 unique hospital admissions included in the cohort, 20,171 (2.7%) of White, 1,913 (2.3%) of Black and 1,062 (2.2%) of Hispanic patients underwent IHT (Figure 1). Patient characteristics differed by race; most notably, compared to White patients, Hispanic patients had a high frequency of Medicaid co-insurance (17.9 vs. 62.1%, respectively). In unadjusted analyses, Black patients had a lower odds of transfer to compared to White patients (OR 0.92, 95% CI 0.89-0.95); there was no difference for Hispanic patients. After adjusting for patient characteristics and hospital fixed effects, compared to white patients, Black patients were associated with a lower adjusted odds of transfer (aOR 0.87, 95% CI 0.81-0.92) while Hispanic patients had a higher adjusted odds of transfer (aOR 1.14, 95% CI 1.05-1.24) (Figure 2).
Conclusions: In this nationally representative study of hospitalized Medicare patients, we found that Black patients had a lower odds and Hispanic patients had a higher odds of undergoing IHT for diseases associated with mortality benefit from transfer, even after accounting for differences in patient and hospital characteristics. Our findings suggest that provider bias is potentially contributing to differential treatment by race. Given these results, more research into transfer decision-making and transfer processes is necessary to further understand these observed inequities in IHT.