Background: In a learning healthcare system, data collected as part of routine care is used to fuel innovation and improvement. Predictive models for post-discharge adverse events have relied on data that is available prior to hospital discharge. Post-discharge care (e.g. appointments, phone calls) can be collected from electronic health records and may impact patient risk for post-discharge adverse events. The objective for this study is to examine the association between different types of post-discharge care and unplanned 30-day readmissions using a national, propensity-score matched sample of patients admitted for congestive heart failure.
Methods: This is a national, retrospective case-control study of patients admitted with congestive heart failure from 2012-2014. Cases were patients with an unplanned readmission within 30 days of discharge. The exposures of interest were seven different types of post-discharge care: emergency room visits that did not result in a hospital admission, scheduled primary care appointments, unscheduled primary care appointments, phone calls to primary care, phone calls to a 24-hour triage nurse, phone calls to a telemonitoring nurse, and scheduled cardiology appointments. Using propensity score matching (with nearest neighbor), patients were matched in a 1:2 ratio on the following: age, gender, Charlson comorbidity index, ejection fraction, number of hospitalizations in the past year, and index admission facility. Because readmission would impact the number of days that cases would be able to access post-discharge care, we developed separate case-control studies for four different post-discharge time periods in which all cases and controls included in that time period were outpatients: 1) discharge to day 3 post-discharge, 2) discharge to day 7 post-discharge, 3) discharge to day 14 post-discharge, and 4) discharge to day 21 post-discharge. This was done to ensure an equal opportunity to access post-discharge care of the cases and controls. We used Fisher’s Exact Test to determine the association between each type of post-discharge outpatient encounter and unplanned readmissions.
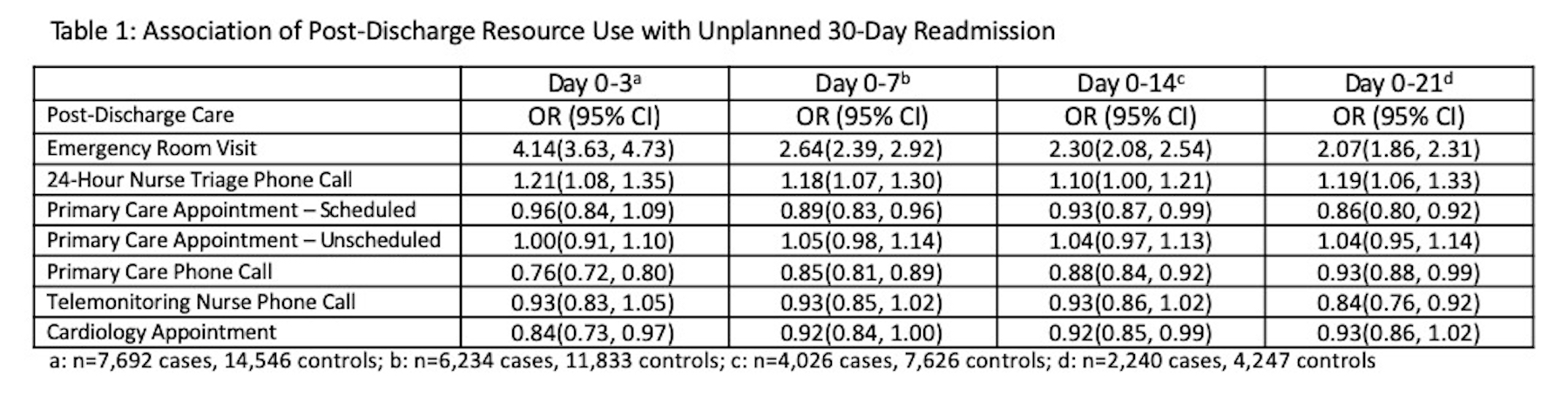
Results: There were 24,435 matched index admissions meeting the inclusion criteria (8,145 cases and 16,290 controls). The mean age was 72.2 years (11.1 SD) in the cases and 72.6 years (11.2 SD) in the controls. The mean number of hospitalizations in the year prior to the index admission was 2.1 (2.6 SD) in the cases and 1.9 (2.2 SD) in the controls. Emergency room visits and phone calls to a 24-hour triage nurse in all four time periods were associated with an increased risk for an unplanned 30-day readmission (Table 1). Scheduled primary care appointments (Day 0-7, Day 0-14, and Day 0-21), primary care phone calls (all four time periods), telemonitoring nurse phone calls (Day 0-21), and cardiology appointments (Day 0-3 and Day 0-21) were associated with a reduced risk for unplanned readmission
Conclusions: Relying on data collected prior to discharge to build predictive models is insufficient to provide real-time assessments of patient risk for readmission in a learning healthcare system. Emergency room visits that do not result in admission or phone calls to a 24-hour triage nurse are associated with an increased risk for readmission in the 30-days following discharge and may be important variables for identifying patients in need of more intensive post-discharge follow-up and monitoring.