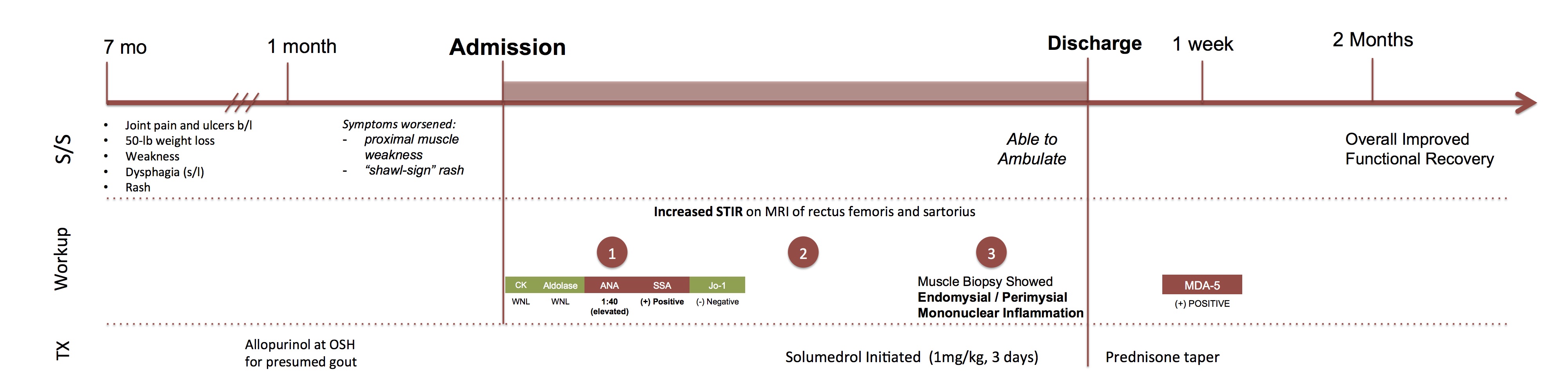
Case Presentation: A 50 yo Hispanic male with a history of Diabetes Mellitus Type 2 and hypertension presented to our hospital with seven months of joint pain and ulcers of his metacarpals, 50-pound weight loss, weakness, dysphagia, and rash. The patient first sought medical attention when he acutely developed severe arthralgia involving his hands. He went to a clinic where he was presumptively diagnosed with gout, and treated with allopurinol. Allopurinol did not relieve his pain, and patients’ symptoms worsened, prompting him to go to LAC+USC Medical Center.
Rheumatology was consulted because serum CK and Aldolase levels were normal despite proximal muscle weakness and characteristic “shawl-sign” rash. ANA (1:40) and SSA were positive, while JO-1 was negative. On imaging, MRI showed increased STIR signal of the rectus femorus and sartorius muscles bilaterally. EMG showed mild myopathic changes in the proximal muscles. CT of chest, abdomen, and pelvis was unremarkable. The patient received 1 mg/kg of Solumedrol for 3 days and began a steroid taper. Muscle biopsy of the right quadriceps confirmed dermatomyositis with prominent atrophy of type 2 fibers and scattered mononuclear cells within endomysial and perimysial connective tissue. At this time, the myositis panel indicated the presence of Melanoma differentiation-associated gene 5 (MDA-5.) Patient regained enough strength to walk, and was discharged with a steroid taper and plans to start a steroid-sparing agent.
Discussion: Diagnosing MDA-5 Dermatomyositis can be difficult because serum Aldolase and CK are often normal. Thus recognizing the characteristic phenotype is crucial—20% of patients with dermatomyositis are amyopathic with skin manifestations predominating. The work-up should include a myositis panel, an EMG or MRI. Muscle biopsy confirms diagnosis. These patients should be closely monitored on an outpatient basis due to the high risk of developing interstitial lung disease.
Conclusions: Dermatomyositis is an idiopathic inflammatory myopathy characterized by proximal muscle weakness and skin manifestations. These patients often have specific autoantibodies that correlate with distinct clinical phenotypes. MDA-5 antibodies are associated with a specific constellation of findings that includes Gottron’s papules, painful palmar macules and papules, alopecia, rash, oral ulcers, arthritis, and amyopathic disease. This is an important clinical entity to recognize due to lack of evident muscle inflammation.