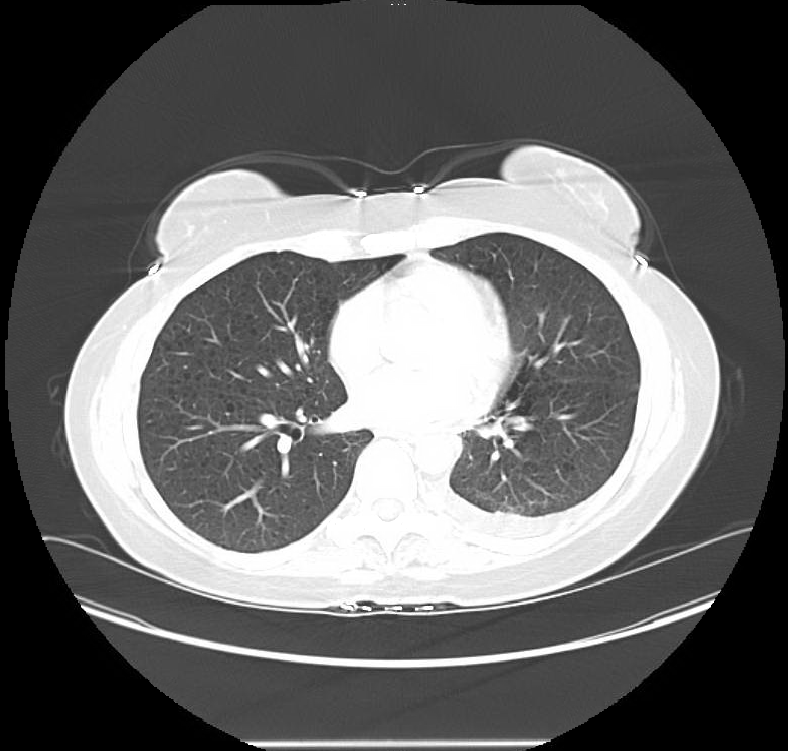
Case Presentation: A 41-year-old female presented with non-productive cough and worsening exertional shortness of breath for 3 weeks. She denied fever, night sweats, orthopnea, paroxysmal nocturnal dyspnea. There was no history of recent travel, smoking, or illicit drug use. She did not have any significant past medical or family history. On physical exam, there was dullness to percussion and diminished breath sound on the left side. Basic blood work including complete blood count and serum chemistry were within normal limits. Chest x-ray confirmed a large left sided pleural effusion. A Computerized tomography (CT) scan of the chest done for further workup revealed numerous thin-walled small cystic lesions in bilateral lung fields along with a large left sided pleural effusion. The patient underwent diagnostic as well as therapeutic thoracentesis. One liter of milky fluid was removed by thoracentesis. Pleural fluid analysis showed lymphocytic predominance (68%), and had a triglyceride level of 2363 mg/dL. Cytology and flow cytometry of the pleural fluid was negative for malignant cells and lymphoproliferative disorders respectively. Based on the clinical presentation and radiological findings, a diagnosis of lymphangioleiomyomatosis was made. Serum vascular endothelia growth factor-D levels were also tested, and came back at 2000 pg/mL. The patient reported of doing better within a week of starting treatment with sirulimus, and has not had a recurrence of her effusion since then.
Discussion: There are two types of LAM- sporadic LAM (S-LAM) and LAM associated with tuberous sclerosis complex (TSC-LAM). TSC-LAM usually present with TSC manifestations along with a positive family history of TSC. A confident clinical diagnosis can be established when typical cystic changes of LAM are seen in high resolution CT and accompanied by any of the following: renal angiomyolipomas, chylous pleural effusions or vascular endothelial growth factor (VEGF)-D level >800 pg/ml. VEGF-D level also helps in correlating with the disease activity. If clinical suspicion remains positive without meeting the criteria described above, lung or lymph node biopsy gives definitive diagnosis. Sirolimus, an mTOR kinase pathway inhibitor, is the current drug of choice for LAM. Sirolimus acts by preventing abnormal cell proliferation. Patients are monitored at regular interval with pulmonary function test for progression of the disease, which most of the time shows obstructive picture.
Conclusions: Lymphoangioleiomyometosis (LAM) is a rare multi-system disease and mostly affects women of child-bearing age, with prevalence of 1 to 3 per million women. LAM is characterized by growth of abnormal muscle-like cells which destroy normal lung tissues resulting in cystic remodeling of the lung parenchyma. LAM usually manifests with exertional shortness of breath, pneumothorax and recurrent chylous pleural effusion. Estrogen exacerbates LAM. Hence, women of childbearing age with LAM, should be informed of complication from LAM during pregnancy.