Background: Simulation-based procedural training has been shown to improve provider competency and confidence in number of medical specialties, including hospital medicine. To the present, simulation training has largely focused on medical students and residents. Attending hospitalists are a prime target for simulation-based procedural training. Despite recent studies showing patient safety and cost-effectiveness of procedures performed by hospitalists, the number of attending hospitalists performing inpatient procedures has been decreasing. This has been attributed to multiple factors including competing time demands, increasing numbers of dedicated proceduralists, and the desire to optimize practice opportunities for trainees. The dearth of opportunity for attending hospitalists to perform procedures limits both the maintenance of independent skills and the ability to fulfill hospital credentialing and privileging requirements. A further challenge to skill building is posed by a common privileging practice that relies on chart review as opposed to direct observation of procedure performance, limiting the opportunity for timely and relevant feedback.
Purpose: To design and implement a convenient, high yield, simulation-based procedure curriculum for hospital medicine faculty, which incentivizes participation by fulfilling hospital procedure privileging.
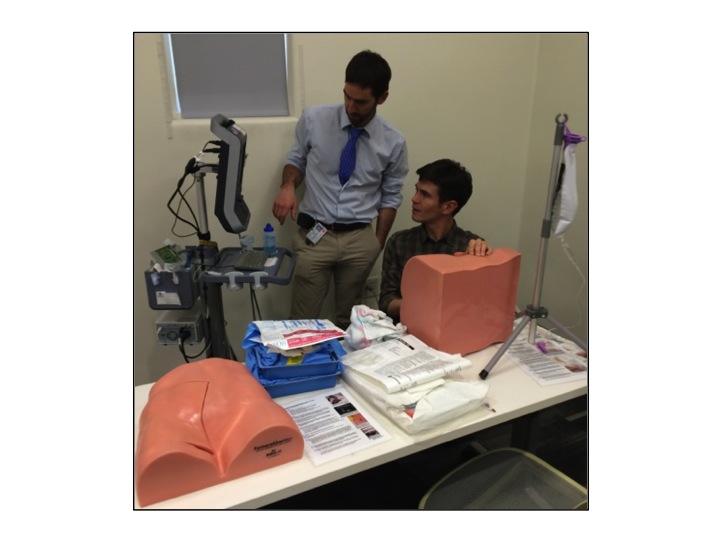
Description: Grant funding was used to purchase high fidelity, ultrasound-compatible simulator models. Literature review was performed to design evidence-based procedure teaching diagrams and rubrics for competency testing. The University of California San Francisco (UCSF) Department of Family and Community Medicine and Department of Internal Medicine obtained approval from the San Francisco General Hospital (SFGH) Credentialing Committee to use supervised, high-fidelity simulator-based procedures to fulfill faculty privileging requirements for lumbar puncture, thoracentesis, paracentesis, internal jugular and femoral CVC insertion. The authors supervise group workshops and individual competency testing for faculty, which include real-time feedback based on existing evidence-based practice. Since initiation of the faculty procedure curriculum in January 2015, 40% of SFGH core medical hospitalist faculty (19/47) have completed training and competency testing through the curriculum. 10 providers have completed 18 discrete simulation-based procedures in order to fulfill hospital privileging. Quantitative surveys of participants show increases in provider confidence for each procedure, and the aggregate mean confidence for all procedures on a 5-point Likert scale increased from 2.7 before training to 4.3 afterwards. Curriculum participants noted a high likelihood, 4.5 on a 5-point Likert scale, of procedure incorporation into practice, and reported reduction in anxiety associated with the procedure, appreciation for the opportunity for practice in a safe space, and increased familiarity with equipment.
Conclusions: We designed an evidence-based, high-yield faculty curriculum for procedure competency using simulation models, which fulfills procedure privileging requirements. Uptake in the first nine months has been excellent and providers report increased confidence following training and a high likelihood of procedure incorporation into practice. Open-source curricular material is provided for use at other institutions.