Background:
Consultative medicine is an important part of Internal Medicine (IM) resident education. According to the Accreditation Council for Graduate Medical Education, residents are expected to “act in a consultative role to other physicians and health professionals.” However, individual programs each have the ability to integrate the consultative experience into training in their own unique ways. Our study details consult rotation structures at a nationally distributed sample of IM residency programs. Such information can inform other programs as to how to develop or improve their own consultative medicine rotations.
Methods:
We describe details of the consult rotations at the affiliate hospitals of various IM residency programs. We included programs from a diverse representation of regions as well as type of hospital. Hospitalists at each site submitted details of their consult services via an online survey, followed by semi-structured telephone interviews to obtain additional details.
Results:
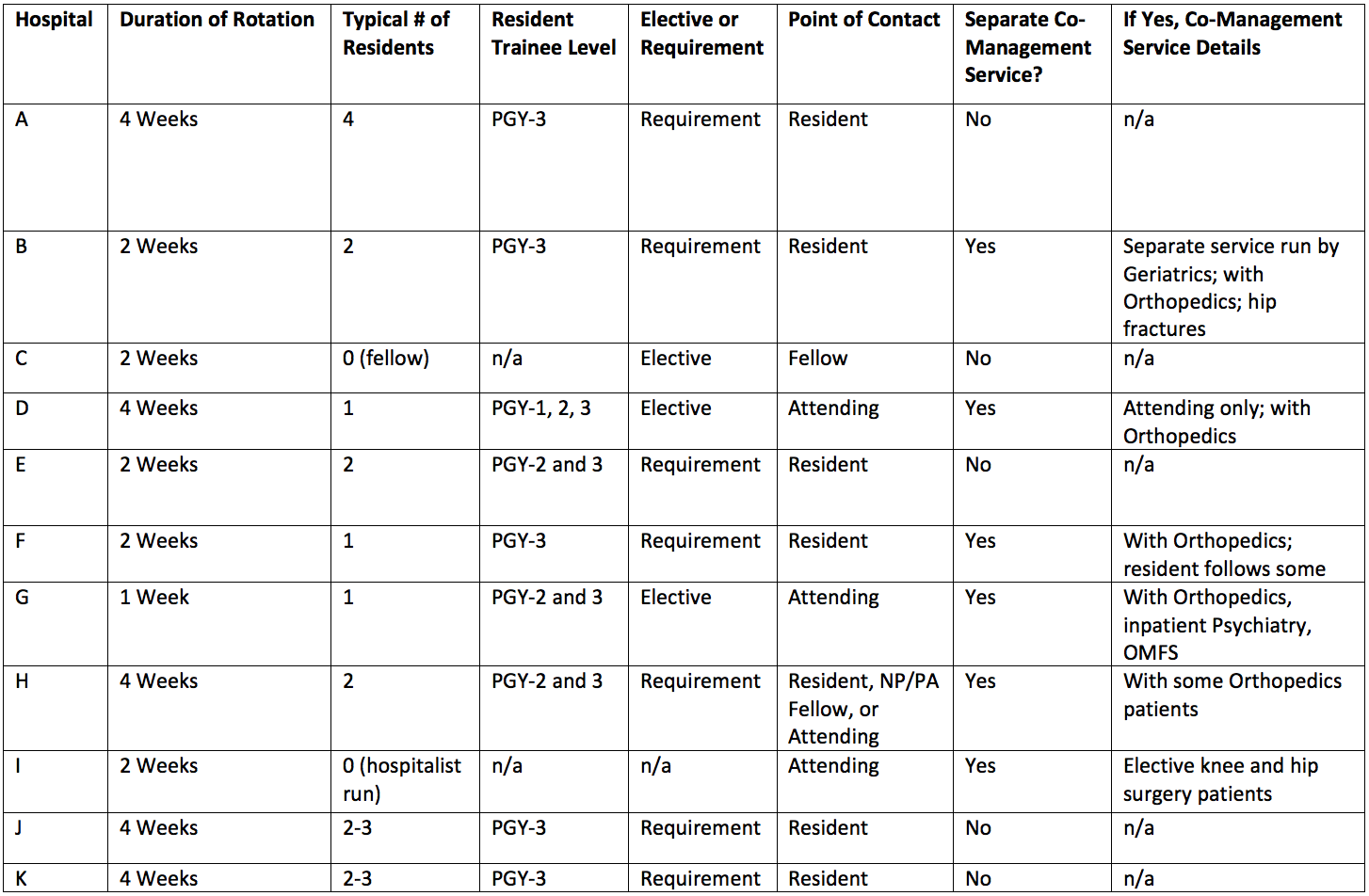
Eleven hospital sites participated, representing nine academic affiliations: two in the Northeast, four in the South, one in the Midwest, and four in the West. Seven hospitals operate as public nonprofit, three as private nonprofit, and one as a Veteran’s Administration hospital. Characteristics of the consultation services at individual hospitals were variable (see Table 1), including two hospitals at which residents were not involved (one in which all consults were seen by hospitalists and another in which all were seen by fellows). Rotation length varied from one to four weeks.
Of the nine sites with resident involvement, the rotation was limited to third-year residents at five sites; to second- or third-year residents at three sites; and to residents of any year at one site. One to four residents rotated on service at a time, with one or two residents being most common. The rotation was required at seven programs and was an elective at two. At six sites, residents were always the first point of contact; elsewhere, attendings could be or always were the first point of contact. Six of the eleven total institutions had a separate co-management service, five of which involved Orthopedic Surgery patients. Residents were often not involved in these co-management services.
Conclusions:
The structure of learners’ consultative medicine experience varies across affiliate hospitals of different IM residency programs. Some more common features include requiring the consult rotation for residents, rotating one to two residents at a time (particularly upper-level residents), and assigning residents with the responsibility of receiving consult requests. These data can provide other programs with a variety of models upon which to base their consultative medicine rotations.