Background: Developing effective tools which enhance patient-physician communication is crucial to improving the patient experience. Existing research has shown that there are several components which are central to effective communication, including creating a good interpersonal relationship, facilitating exchange of information, and including patients in decision making. Based on our experience at an underserved community hospital in the South-Central Bronx, barriers to effective patient-physician communication include limited health literacy, varied levels of patient engagement, and an inconsistent approach to training physicians on how to provide information to patients regarding aspects of their care.
Purpose: We present the design and implementation of a scripted communication tool aimed to positively affect doctor-patient communication, in a user-friendly way.
Description: A literature review was conducted to identify best practice components of an effective physician-patient encounter. Focus groups incorporating physician and patient views were used to identify specific areas for improvement. A scripted communication checklist tool was developed, implemented, and measured for effect using PDSA rapid cycle improvement methodology, to create a tool that was easy to implement, did not impede physician workflow, and improved patient-doctor communication and patient awareness during their hospital course.
The G’NITE Check-list
Greeting (Hello, nice to meet you, I am..)
New medications/treatments (I wanted to update you on new medications/treatments planned..)
Information (I have the following test/consult results for you..)
Tomorrow (Here’s what we have planned for tomorrow..)
Expectations (Are you in any pain? Is there anything else that I can do for you?)
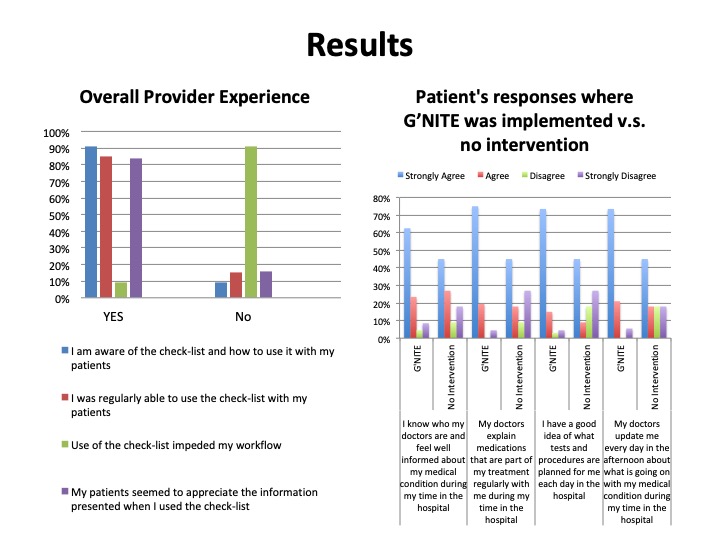
Baseline patient experience data was collected and reviewed on three similar inpatient medicine units, with one unit subsequently selected as a control unit, and two units identified for comparison following the planned intervention. Four PDSA cycles were conducted over 10 weeks, during which staff on selected units were trained, physician champions were engaged, and performance regularly monitored. Each patient care list (12-15 patients) was divided up daily in the afternoon (attending/resident/2 interns), and a focused encounter, lasting 5-7 minutes per patient, was implemented using the scripted communication tool checklist. Resident experience with the tool was measured by self- report, and patient experience was measured independently by patient relations staff, with more than 30 unique residents and 90 unique patients surveyed.
Conclusions: Patients surveyed on the units where the checklist was implemented felt better informed about their health issues, and had a good understanding of the tests and procedures planned for them in the hospital, compared to the control unit. Providers surveyed on the selected units felt that the checklist was easy to use, provided benefit to their patients, and did not impede their workflow. From our experience, implementation of a scripted communication checklist tool has significant opportunity to help minimize variability, enhance routine patient-physician communication, and improve the patient experience within the hospital setting.