Background: One of the challenges in hospital medicine is the effective and efficient evaluation of patients through the emergency department and admission. When this does not work well we see long wait times in the emergency department, patients leaving without being seen and decreased patient satisfaction. In the extreme case, we see ambulance diversion. This is a difficult problem to address because there are so many steps between emergency department arrival and transfer to the inpatient ward. The timepoints in this process that can be measured are emergency department arrival, evaluation by emergency department provider, decision to admit by emergency department provider (ADT9), bed request order by admitting provider (ADT1), bed assignment and emergency department departure. We felt that as hospitalists, we have the greatest ability to impact the time from the decision to admit to the bed request order being placed (ADT9-ADT1).
Purpose: Attempt to reduce the ADT9-ADT1 time for hospitalist patients, thereby reducing ADT9-emergency departure times and overall emergency department length of stay.
Description: From July 2017-June 2018, the hospitalist team tied a financial incentive to a target ADT9-ADT1 time of 60 minutes. Individual hospitalist ADT9-ADT1 times were measured over the year and emailed to the entire team on a monthly basis, so that each provider could see how they compared to the rest of the group. Of note, each hospitalist’s data was also made available to non-hospitalist providers.
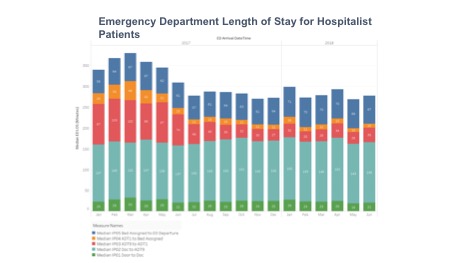
The ADT9-ADT1 time for hospitalist patients decreased from a baseline of 93 minutes to 48 minutes just one month after these changes. (graphic 1) Additionally, the median ADT9-ADT1 time from July 2017-June 2018 was 33 minutes, which is a 65% reduction from the prior six months.
Prior to our intervention, the median ADT9-emergency department departure time from January to June 2017 was 184 minutes, higher than both the national and North Carolina medians. After our intervention, the median ADT9-emergency department departure time from July 2017-June 2018 decreased to 110 minutes, lower than the national median of 120 minutes and the North Carolina median of 110 minutes.
Conclusions: Not only was there an immediate improvement in emergency department throughput, but the results were sustained throughout the year. These results show the potential impact of a financial incentive and data transparency. Future projects may look at the impact of our work on HCAHPs scores and ambulance diversion hours.