Background: Heparin-Induced Thrombocytopenia (HIT) is an antibody-mediated pro-thrombotic disorder which occurs after exposure to heparin product. Diagnosis of HIT type II is rather challenging as affected individual often has other causes of thrombocytopenia and a delayed discontinuation of heparin in HIT type II is associated with a mortality rate of 20-30%. 4Ts score is a validated screening tool with a high negative predictive value in excluding HIT type II when a low probability score is present. Hence, this clinical scoring system (4Ts) was adapted by our hospital in November 2014 as an effort to reduce the number of inappropriate HIT antibody testing. The aim of this study was to assess the outcomes of pre- and post-implementation of the 4Ts scoring system.
Methods: We conducted a retrospective chart review of patients who had HIT antibody tests ordered. There was a pre-intervention phase (January 2013 – June 2014) which served as a control, and a post-intervention phase (August 2015 – February 2017) which served as a comparison. Pre-intervention: A total of 154 patients had the HIT antibody testing ordered prior to the hardwiring of the 4Ts scoring system in the EMR. Then, there was an extensive in-house education provided to the healthcare providers regarding the need of completing 4Ts score prior to ordering the HIT antibody tests over the 13 months period. Post-intervention: A total of 103 patients had the HIT antibody testing ordered after the 4Ts scoring system was created in the EMR. Inclusion criteria: Patients who were suspected to have HIT type II and HIT antibody tests sent out. Exclusion criteria: Age under 18-year-old. The number of 4Ts scores documented and the appropriateness of HIT antibody tests ordered between pre- and post-intervention were compared.
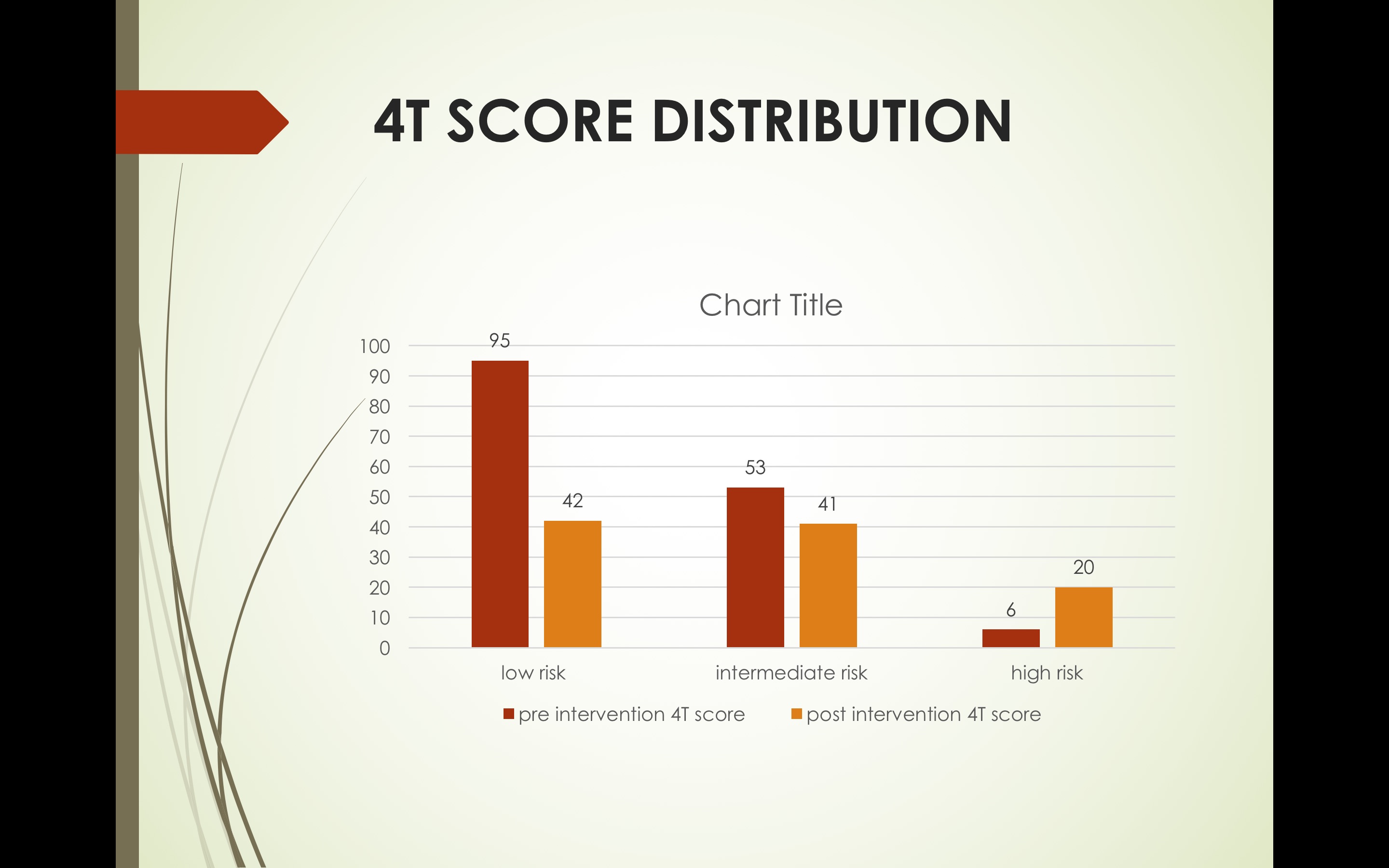
Results: Pre-intervention, only 1.3% (2/154 patients) had their 4Ts score documented in the chart, which significantly improved to 34% (35/103 patients) post-intervention [1.3% vs 34%, p < 0.00001]. Pre-intervention, 62.3 % (95/154 patients) with low probability score had unnecessary HIT antibody testing ordered, which significantly reduced to 40.8% (42/103 patients) post-intervention [62.3% vs 40.8%, p = 0.00068]. The total average cost of HIT antibody testing per patient was around $5,000. As the test takes 3 – 5 days to return, the average length of stay in hospital ($7,000/day) will inadvertently be prolonged. Hence, if the physician complies with the use of 4Ts score, an estimated cost savings per patient is between $26,000 - $40,000.
Conclusions: It is evident that the implementation of the 4Ts scoring system in EMR had significantly reduced the number of inappropriate HIT antibody testing in low probability group. Clinicians are encouraged to utilize the 4T scoring system prior to sending HIT panels to reduce unnecessary testing and practice cost-effective medicine.