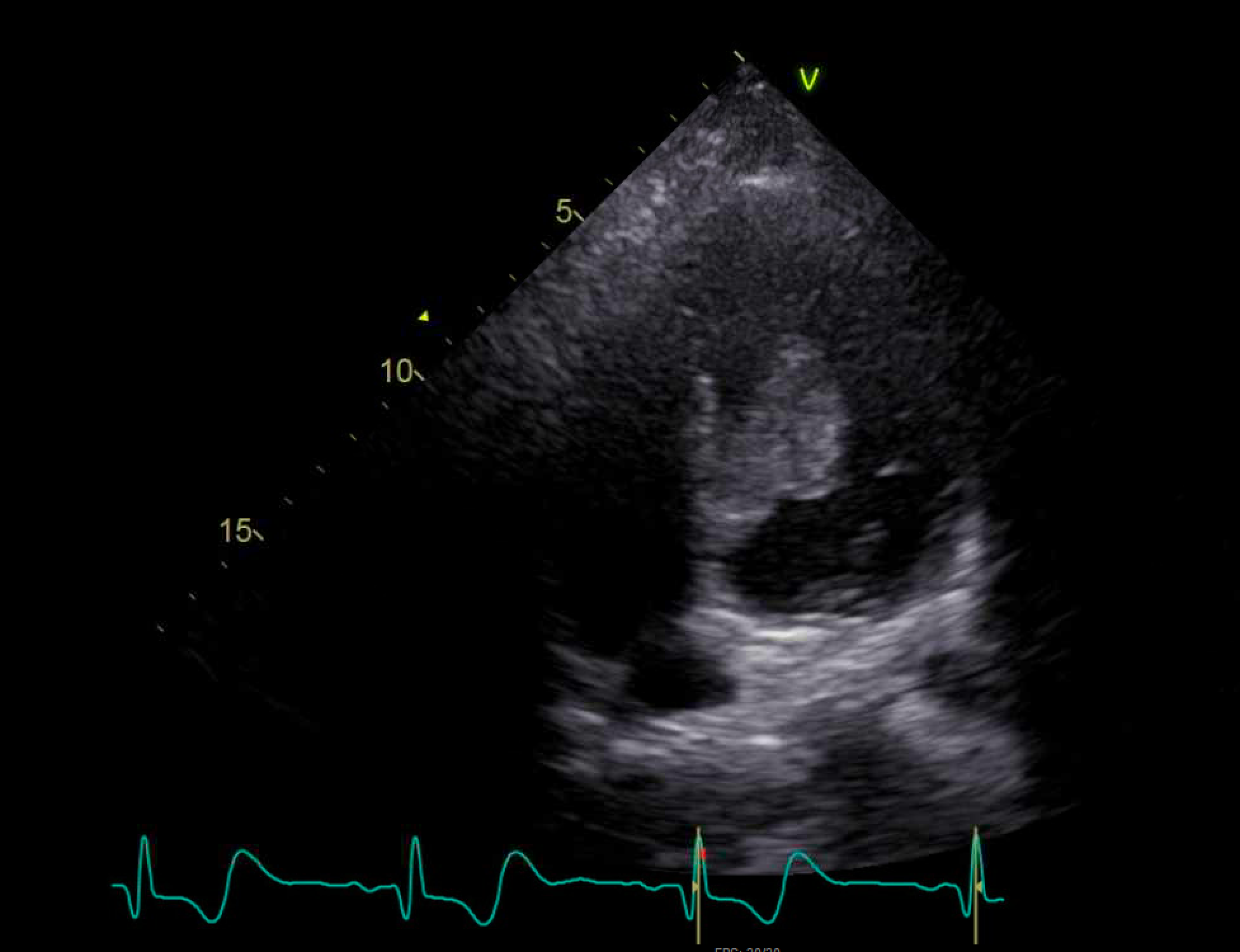
Case Presentation: A 22-year-old previously healthy man presented to the emergency department with sudden onset left flank pain that began shortly after shoveling his driveway and radiated to his groin. He noted mild dyspnea while shoveling but otherwise denied urinary or constitutional symptoms. His physical exam was notable for fever with a temperature of 38.2C, tachycardia with a heart rate of 105 bpm, and costovertebral angle tenderness on the left. Initial laboratory studies revealed leukocytosis (WBC 18.9 x 10^9/L) and an unremarkable urinalysis. CT abdomen/pelvis with contrast demonstrated a “striated nephrogram” appearance of the left kidney, further interpreted as “most likely representing pyelonephritis” (Fig 1). He was treated with a dose of intravenous ceftriaxone and admitted to hospital medicine. After independently reviewing the CT images, the admitting team ordered a transthoracic echocardiogram (TTE) as part of an embolic work-up, which demonstrated a large tissue-density mass in the center of the left ventricular (LV) cavity (Fig 2). Cardiac MRI confirmed the presence of a large LV mass involving much of the cavity with extension along the papillary muscle and mitral valve. Pathology from an LV biopsy revealed the diagnosis of synovial sarcoma.
Discussion: Primary cardiac synovial sarcomas are highly aggressive, predominantly right-sided tumors that account for only 0.1% of all malignant primary cardiac tumors. Although a left-sided cardiac synovial sarcoma is an exceptionally rare diagnosis, all hospitalists will encounter patients with undifferentiated hyperacute symptoms. The time course of illness is a critical aspect of one’s diagnostic reasoning in these cases as it prioritizes certain pathologies including vascular phenomena such as thromboembolism. Signs of inflammation, radiologic findings, and the initiated treatment plan for pyelonephritis created robust diagnostic momentum frequently seen during the admission process. However, when the admitting team independently reviewed the CT images through the lens of this patient’s hyperacute symptom onset, they favored a diagnosis of inflammation secondary to renal infarct. A consulting radiologist confirmed that the striated appearance of the kidney could also be consistent with infarct. TTE revealed a large LV mass suggestive of either benign vs malignant tumor, thrombus, or less likely atypical endocarditis. Cardiac MRI was essential in determining the extent of the mass and the invasive nature, further supporting the diagnosis of a cardiac tumor.
Conclusions: This case utilizes an atypical presentation of a rare cardiac tumor to highlight the importance of key aspects of the diagnostic reasoning process: the prioritization of the tempo of disease in one’s problem representation and independently reviewing imaging studies through the lens of the clinical presentation. The admitting team recognized the discordance between key features of the clinical picture and the working diagnosis on admission of pyelonephritis. They importantly did not solely rely on the interpretation of the CT study, but independently reviewed the images and utilized a consulting radiologist for a second opinion. This diagnostic tension prompted the consideration of renal infarct and the pursuit of further studies investigating potential sources of embolization, ultimately revealing a large cardiac mass. Without this intentional diagnostic reasoning, the patient’s cardiac mass may have been missed.