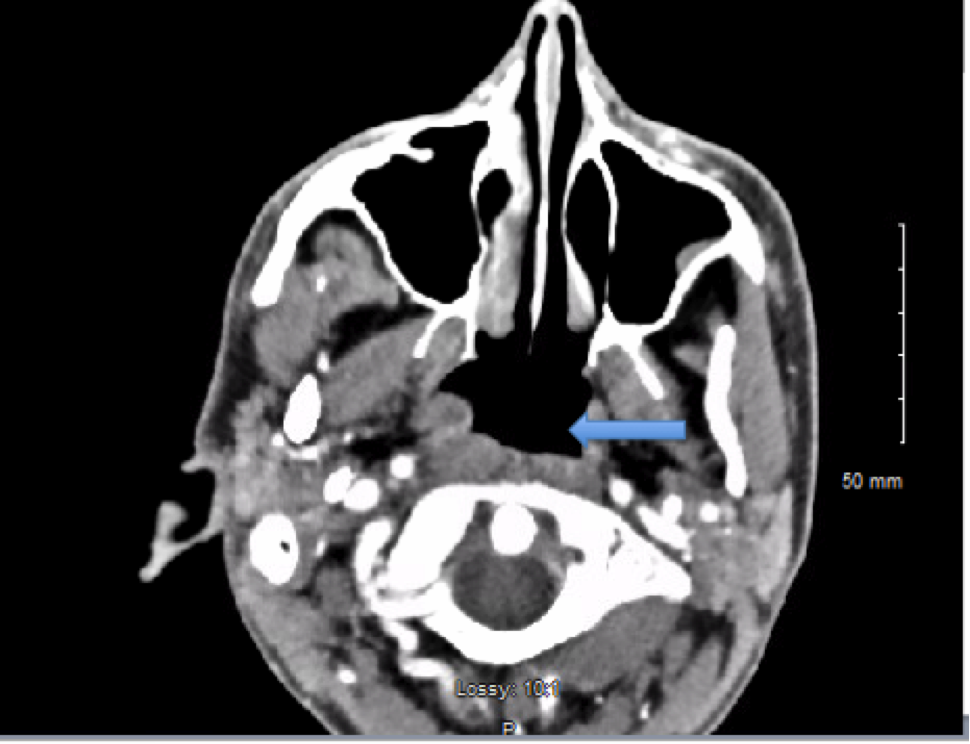
Case Presentation: A 41-year old male with history of alcohol abuse and polysubstance abuse, presented after being found unresponsive on the floor. He had been complaining of nausea, vomiting and abdominal pain. The patient was noted to have blood around his mouth, was cyanotic appearing with dilated unresponsive pupils. He was emergently intubated and started on norepinephrine drip. He had a temperature of 33.7oC, blood pressure of 74/61 mmHg, pulse of 58/min, respiratory rate of 13/min. Laboratory results showed leukocytes of 16.9 x10 (3)/mcL, bands of 9%, creatinine of 1.92 mg/dL, and lactic acid of 14.5 mmol/L with a PH of 7.032. There was detectable alcohol level in the blood. Physical exam was remarkable for poor dental hygiene. CT of the chest showed bilateral lower lobe and right middle lobe infiltrates suggestive of pneumonia. The patient was admitted to the ICU for septic shock from aspiration pneumonia. He was started on vancomycin, piperacillin-tazobactam, and doxycycline empirically. The patient’s father later reported that the patient was picking on a gingival abscess for a period of time. Subsequently, maxillofacial CT scan showed a nasopharyngeal/oropharyngeal abscess measuring 1.6 x 1.0 cm tapering inferiorly for about 3.4 cm (image 1). At this time, the patient’s blood cultures grew Actinomyces odontolyticus. Vancomycin and doxycycline were then discontinued. The abscess was not drained since it was small. The patient continued treatment with piperacillin-tazobactam for a total of 4 weeks; then with oral amoxicillin for a prolonged duration. A follow-up Ct scan (image 2) showed resolution of the abscess after 4 weeks.
Discussion: As with other actinomycotic diseases, Actinomyces odontolyticus is an endogenous infection from the mucous membrane but less encountered than other species. Typically Actinomyces species can cause localized infection at the site of tissue invasion; hematogenous spread is rare and leads to significant morbidity through sepsis response similar to our case. In our patient, the original source of bacteremia was the pharyngeal abscess; bacteremia caused septic shock and serious disease. Additionally, the presence of Actinomyces in blood cultures could be transient but if true infection is untreated, it could be fatal. It is important to advise patients to reduce alcohol abuse and improve their dental hygiene to prevent this infection.
Conclusions: Actinomyces bacteremia is rare, but more reported now given modern culture techniques. It is not always meaningful but can be fatal if a true bacteremia is not treated. Hospitalists should be aware to involve infectious diseases consultants to help manage these cases.