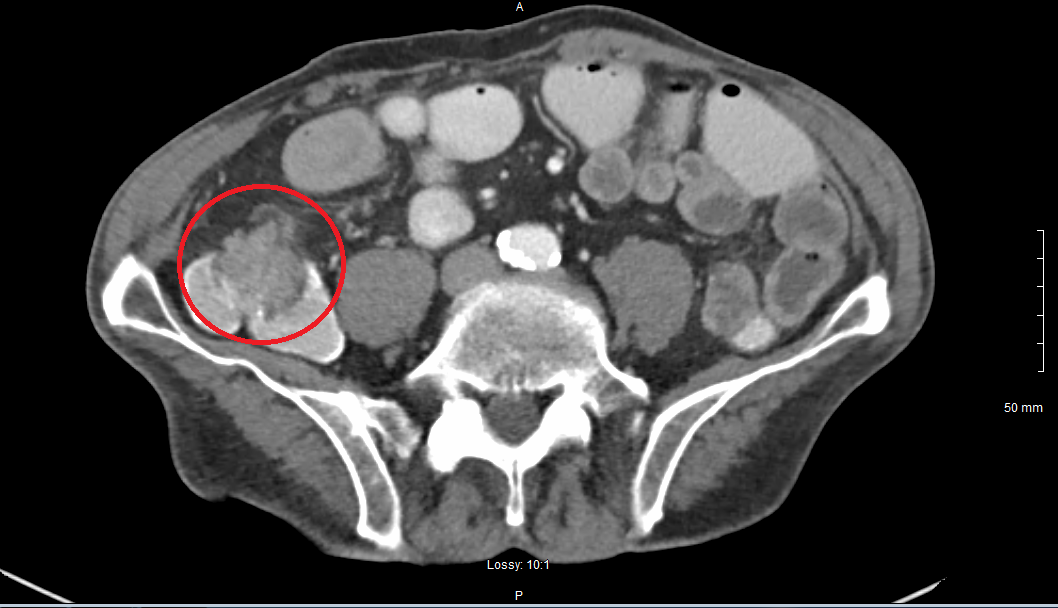
Case Presentation: A 79 year old male presented after having recurrent falls. He was extremely weak, and reported that he had lost about 20 lbs in the past month. The patient’s family reported a significant decrease in his appetite. Past medical history included COPD, CAD status post CABG, and CVA. In the Emergency Room the patient had a temperature of 36 oC, pulse of 136, respiratory rate of 16, and a blood pressure of 96/66 mmHg. EKG showed atrial fibrillation in rapid ventricular response. Laboratory studies were remarkable for leukocytosis of 17.5 with 12% bandemia, AKI with BUN/Creatinine of 35/1.60, and procalcitonin of 0.46. He was admitted for severe sepsis due to possible community acquired pneumonia complicated by new-onset atrial fibrillation. Ceftriaxone and Doxycycline were started. CT Chest did not show any clear signs of pneumonia. Blood cultures from admission grew S. viridans. Infectious disease was consulted and recommended continuing Ceftriaxone. Echocardiogram showed no signs of valve vegetation. He developed constipation, nausea/vomiting and abdominal pain; his hemoglobin level was also found to be down-trending, from 10.3 g/dL to 7.9 g/dL. A CT abdomen/pelvis showed distal small bowel thickening, suggestive of infectious vs inflammatory, but a mass could not be excluded. He has never had a colonoscopy. Gastroenterology was consulted, and colonoscopy showed a cecal mass on the ileocecal valve with invasion of the terminal ileum. General surgery was consulted for right hemicolectomy for obstruction. Pathology confirmed the mass to be adenocarcinoma, with lymph nodes positive for metastasis. Oncology was consulted and chemotherapy was discussed. Ceftriaxone was discontinued after total 14 days from the last negative blood culture.
Discussion: Colonic malignancy associated with S. bovis/galloyticus is well documented in literature, but very few case reports document other streptococcal species associated with colonic carcinoma. S. viridans is a low virulence organism, and would take impaired host immunity for it to cause a bacteremia. One hypothesis is the tendency of S. bovis to attach itself to surfaces of tumors or an adenoma and with increased inflammation and tissue breakdown would translocate into the circulation causing bacteremia. Further studies will need to be done to see if this is a similar mechanism for the S. viridans group as well. Our patient was in very poor nutritional status, with significant weight loss which could have contributed to his diagnosis. Infective endocarditis is a common finding with S. viridans bacteremia, but our patient did not present with any valve vegetation on echocardiogram.
Conclusions: The association between colonic carcinoma in the setting of Streptococcus bovis biotype I (Streptococcus galloyticus) bacteremia, has been well described. Although not fully understood, one hypothesis is the ability of S. galloyticus to cause colonic inflammation with induction of cytokines and transcriptional factors promoting carcinogenesis. Many are not aware that other streptococcal species can also be associated with colonic carcinoma, and cases are rare. It is important to have an infectious disease specialist involved to guide treatment. The association between S. viridans and colonic neoplasm should be considered when there is bacteremia, as there is potential to find pre-malignant adenomas and treat early.