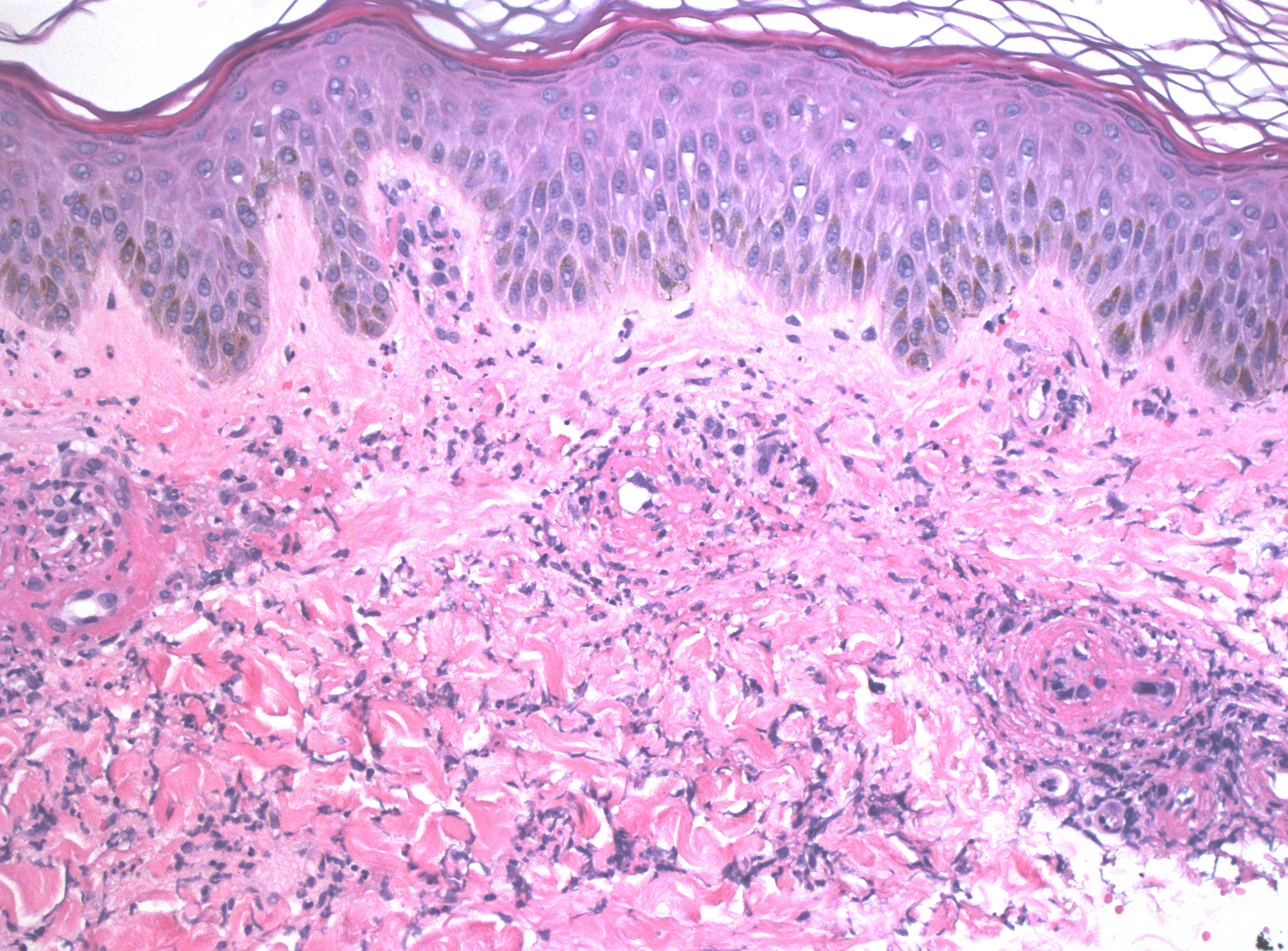
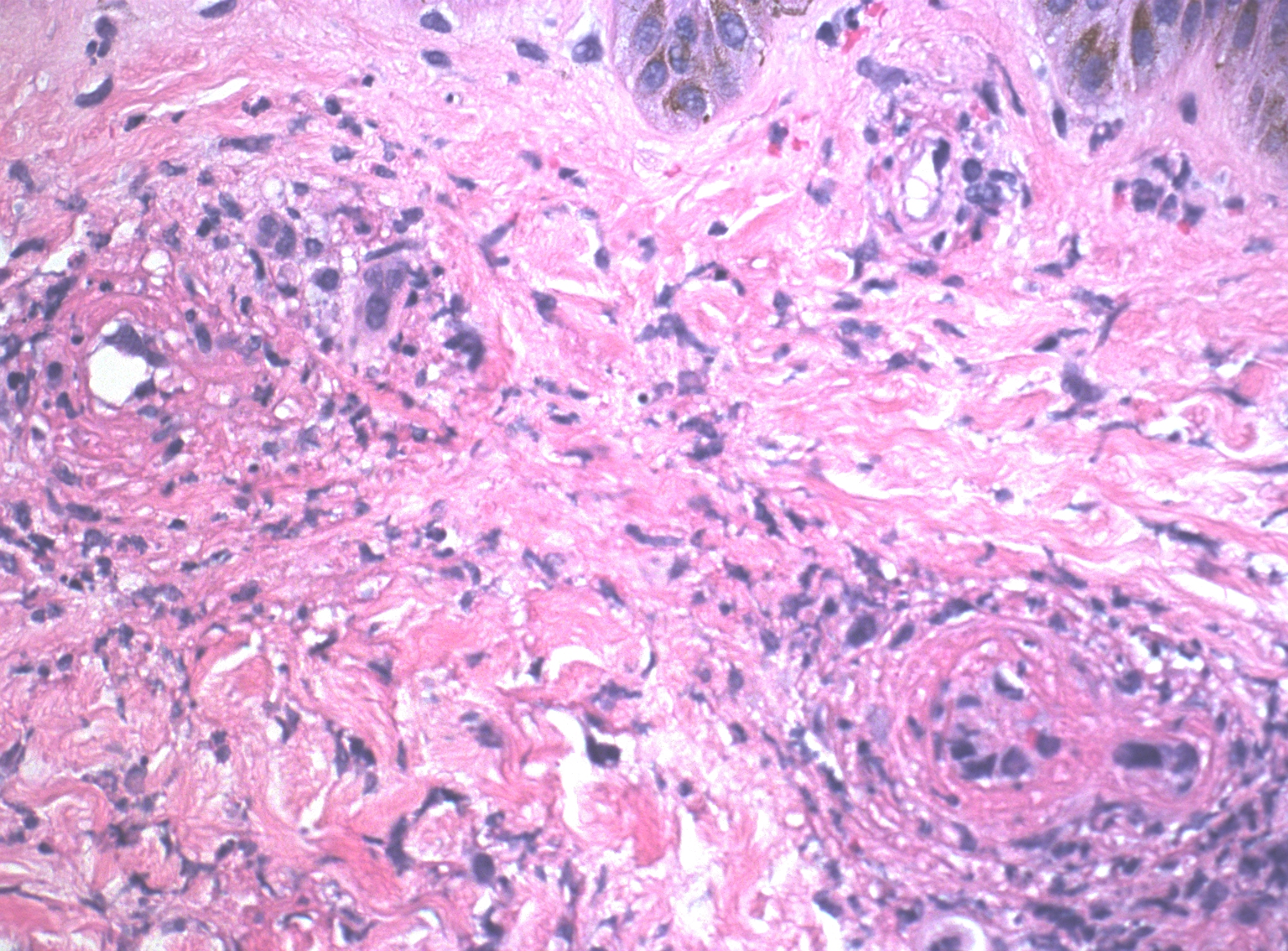
Case Presentation: A 51-year-old female with no past medical history presented with a rash that developed a week ago which started on her right calf and then progressed all over her body. She was on ibuprofen for right knee pain for the 3 weeks before her presentation. Vital signs were normal. Laboratory tests revealed leukocytosis, and elevated inflammatory markers [(erythrocyte sedimentation rate (112 mm/hr), and C-reactive protein (10.54 mg/dL)]. Antinuclear antibodies and qualitative cryoglobulin C returned positive and serum complement protein C3 was elevated (245 mg/dl). Rheumatoid factor, CCP antibodies IGG/IGC, Sjogren’s antibody (anti-SS-A/-SS-B), anti-DNA(DS), serum complement C4, ANCA profile (anti-MPO antibodies, anti-PR3 antibodies, atypical P ANCA) were negative. Thyroid stimulating hormone, creatinine, liver enzymes, prothrombin time, and partial thromboplastin time were normal. Urine analysis showed no proteinuria. Human immunodeficiency virus antibody/antigen test, hepatitis B and C serologies, syphilis screening, and Lyme serology were also negative. The rash evolved from maculopapular purpuric lesions to the development of tender vesicles, bullae, and ulcerations therefore a punch biopsy of the skin was performed, which showed leukocytoclastic vasculitis. Ibuprofen was stopped and the patient was started on a prednisone taper. The eruptions cleared and bullae started healing. The patient was diagnosed with biopsy-proven leukocytoclastic vasculitis with cryoglobulinemia secondary to ibuprofen use. She was discharged on oral prednisone, and topical triamcinolone, and referred to dermatology, and rheumatology, for further evaluation. She reported improvement at her follow-up appointment in the dermatology clinic.
Discussion: This case highlights the importance of considering medication-induced leukocytoclastic vasculitis when evaluating patients who present with unexplained rash. Ibuprofen-induced leukocytoclastic vasculitis is a rare but recognized adverse reaction to ibuprofen involving the drug acting as a hapten and initiating immune complex deposition and activation of the complement cascade in postcapillary venules, resulting in fibrinoid necrosis. Drug-induced eruptions are based on inferential evidence, usually involving a history of ingesting the suspected drug and resolution of the eruption once the drug is discontinued [1]. Diagnosis is dependent on skin biopsy but also relies on a combination of clinical features and exclusion of other causes [2].
Conclusions: This case highlights the importance of a multidisciplinary approach to diagnosing cutaneous vasculitis, especially in the absence of other potential causes such as infections, underlying autoimmune disorders, other drugs, and the association between NSAID use, particularly ibuprofen, and the development of leukocytoclastic vasculitis.