Case Presentation: 64-year-old healthy male was admitted for fever, chills, generalized fatigue and jaundice. Physical exam showed scleral icterus. Lab data showed white cell count of 8.2 k/μL, hemoglobin 15.2 g/dL, and platelets 26,000 cells/μL. Patient also had abnormal LFTs with AST 458 U/l, ALT 227 U/l, Bilirubin 8.3 mg/dl and ALP 160 U/l. Patient was admitted for suspected sepsis and started on broad spectrum antibiotics. Urinalysis was normal and X-ray chest didn’t show any infiltrates. CT abdomen and pelvis showed hepatosplenomegaly. Right upper quadrant ultrasound showed mild hepatomegaly and fatty liver. MRCP showed no evidence of biliary obstruction. Venous portal hepatic venous duplex showed patent hepatic vasculature with no evidence of portal hypertension. During hospital course sepsis work up including blood, sputum and urine cultures remained negative. Echocardiogram showed normal EF without evidence of vegetations. Further lab work showed hyperferritinemia with ferritin of 8350 ng/ml without evidence of iron overload (iron 118ug/dl, iron saturation 46%, transferrin 151 mg/dl and TIBC 259 ug/dl). Serum triglyceride levels were elevated at 356 mg/dl and fibrinogen levels were low 128 mg/dl. Inflammatory markers including ESR,CRP were normal. Autoimmune panel including ANA, antimitochondrial antibody, anti-smooth muscle antibody, anti-LKM antibody were normal. Patient had normal ceruloplasmin and alpha 1 antitrypsin levels. Hepatitis A total and IgM Ab negative, HBsAg and HBsAb negative, Hepatitis C Ab and PCR negative, CMV PCR negative, EBV PCR negative, HSV PCR negative, SARS-CoV-2 PCR negative, HIV 1,2 antigen/antibody test negative. Bone marrow biopsy didn’t show any evidence of hemophagocytosis and peripheral blood flow cytometry was normal however liver biopsy was consistent with hemophagocytic lymphohistiocytosis. Patient met criteria for HLH with fever, splenomegaly hypertriglyceridemia, elevated ferritin and soluble IL-2 receptor hemophagocytosis in liver. HLH mutation panel was negative. Patient during hospital course had spontaneous resolution of fever and transaminitis/hyperbilirubinemia and was discharged with outpatient follow up with hematology.
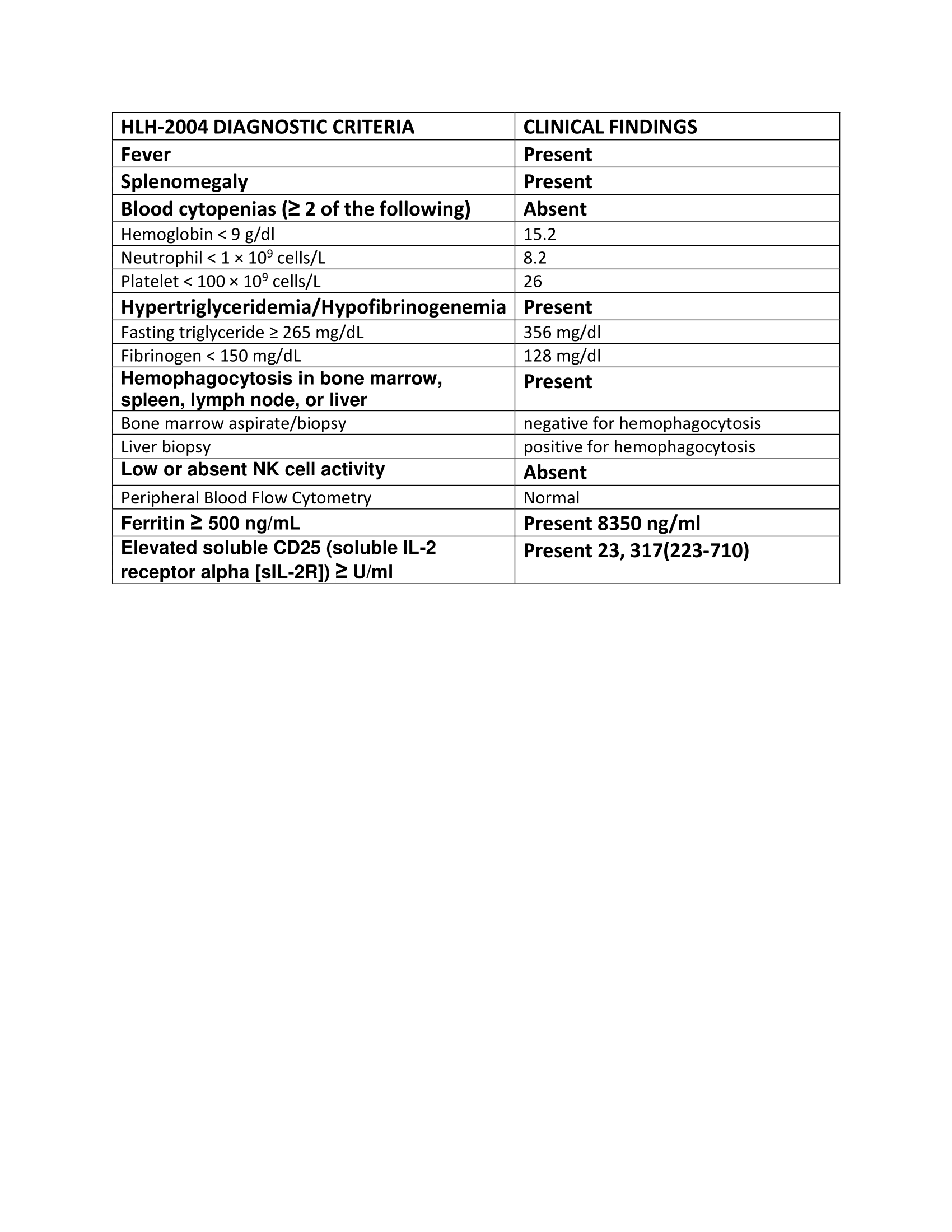
Discussion: HLH is a rare life threatening syndrome of multi organ involvement due to widespread immune response. We present a rare case of idiopathic HLH in adults which was managed conservatively with good outcome. Classification includes primary (common in children) and secondary or acquired HLH (common in adults). Secondary HLH is usually associated with malignancies (leukemia, lymphoma), infections (CMV, EBV, HIV) and autoimmune (SLE) or rheumatological diseases (RA). No underlying disease was detected in our patient after extensive work up. Diagnosis of HLH is based on clinical, laboratory and histopathological findings based on HLH 2004 diagnostic criteria. Our patient met 6 out of the 8 criteria required for diagnosis as shown in Figure 1. Treatment includes corticosteroids and chemotherapy however is based on clinical manifestations and underlying secondary causes. Our patient had one episode with spontaneous resolution without any obvious trigger and was monitored for the next 2 years without any further recurrence.
Conclusions: This case report highlights importance of high suspicion of HLH as diagnosis can be easily missed in adult population due to rare incidence. High mortality associated with HLH requires timely diagnosis using HLH-2004 diagnostic criteria for early initiation of treatment.