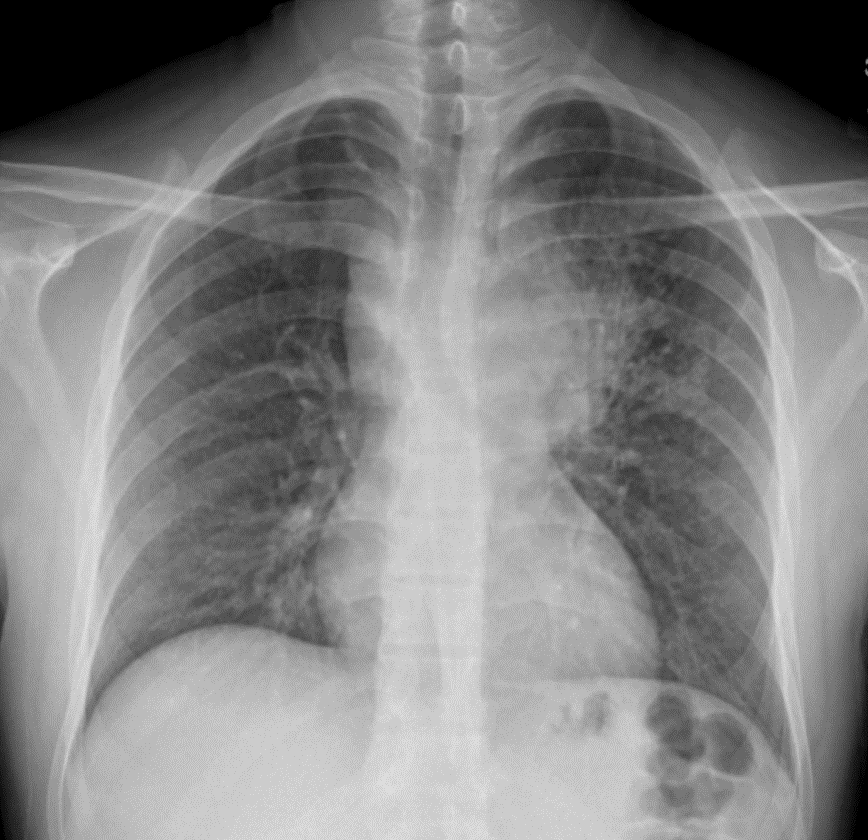
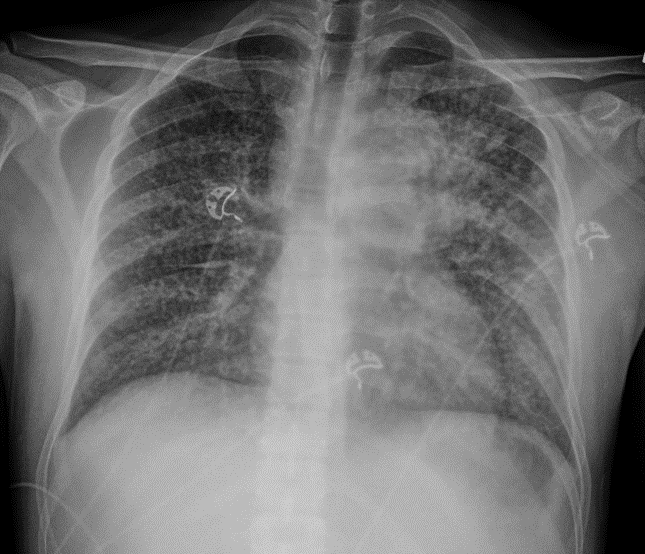
Case Presentation: A 28-year-old male who immigrated from Guatemala six years ago with untreated HIV presented with 3 weeks of fatigue, headache, and night sweats. He was initially diagnosed with HIV three years earlier, but just began ART one week prior to his presentation, after being seen at a community clinic. He was started on dolutegravir and lamivudine, trimethoprim-sulfamethoxazole for Pneumocystis jirovcii prophylaxis, and fluconazole for oral candidiasis. He reported intermittent fevers and chills, but denied chest pain, dyspnea, cough, or abdominal pain. On presentation, he was febrile to 102.7F and tachycardic to 146 bpm. He was diaphoretic, but not in respiratory distress. Labs were notable for a mild leukocytosis of 11.3k, lactic acidosis of 2.6, positive COVID-19 test, CD4 count of 110, and HIV viral load of 2280 copies/mL. Serum cryptococcal antigen was negative. CT chest revealed a large left-sided paramediastinal mass measuring 9 x 4.7 cm with extensive supraclavicular and mediastinal lymphadenopathy, but no lung lesions. On admission, ART was transitioned to dolutegravir, emtricitabine, and tenofovir alafenamide. He underwent bronchoscopy with lymph node biopsies which revealed the presence of acid-fast bacilli consistent with Mycobacterium tuberculosis (TB), but no malignant cells. Therapy was initiated with rifampin, isoniazid, pyrazinamide, and ethambutol (RIPE). On the fifth day of admission, he developed sudden onset tachypnea. CT chest showed new innumerable pulmonary nodules consistent with miliary TB. Concern for unmasked TB-IRIS prompted the cessation of ART. Due to rapid development of liver injury and possible paradoxical phenomenon from antigen release, RIPE therapy was paused and gradually re-introduced incrementally. He improved significantly and was discharged with close follow-up for continued management of his TB and HIV. ART was successfully resumed as an outpatient.
Discussion: Tuberculosis (TB) is the leading cause of morbidity and mortality among people with HIV worldwide. Tuberculosis immune reconstitution inflammatory syndrome (TB-IRIS) is a unique phenomenon that describes an early complication of antiretroviral (ART) therapy in HIV patients with subclinical TB. The initiation of ART restores immune function and consequently exaggerates the immune response to underlying indolent infections, such as TB. Similarly, anti-TB therapy can paradoxically worsen TB infection by weakening encapsulated granulomas and releasing infective particulates, especially in patients with AIDS. The newly “unmasked” TB antigens result in profound inflammatory reactions.
Conclusions: Our patient’s case demonstrated ART-induced unmasking of subclinical TB and a paradoxical rapid progression to miliary TB. This occurs as dysregulated restoration of pathogen-specific immune responses trigger the presentation of asymptomatic diseases. TB-IRIS has historically been a disease of the developing world; however, with recent increased rates of immigration from TB endemic areas, this entity will undoubtedly become more prevalent in the developed world. High-risk patients beginning ART require close monitoring for unexpected disease presentations. Clinically tenuous patients co-infected with HIV and TB require a multidisciplinary approach to optimize treatment and minimize complications.