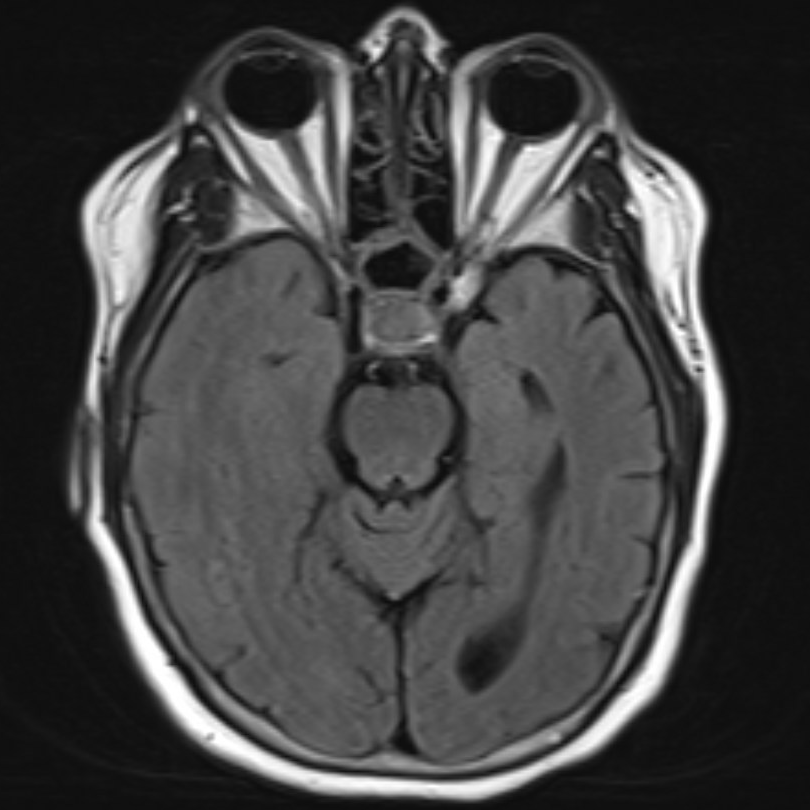
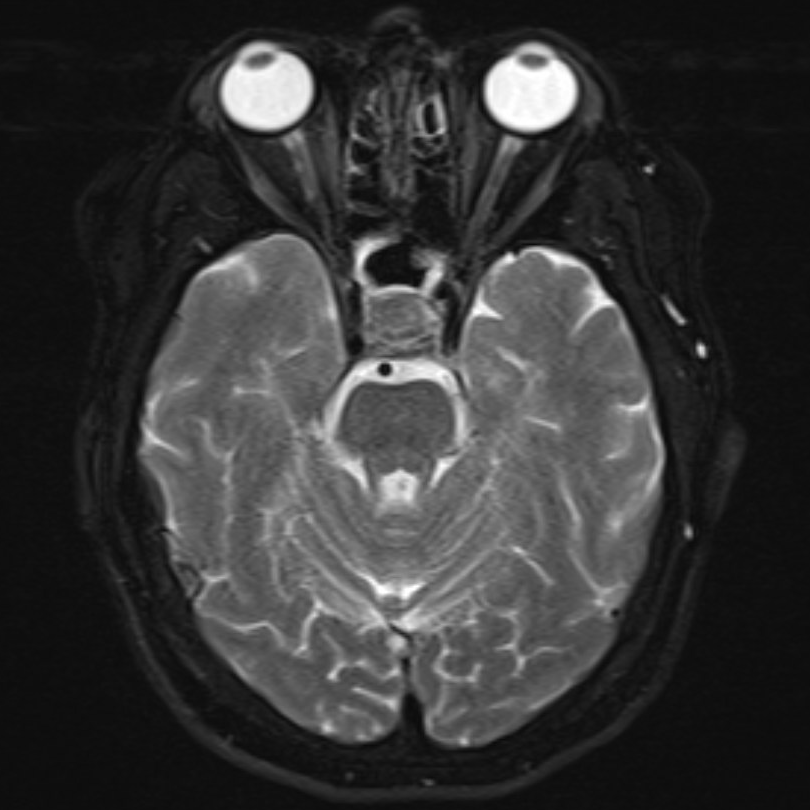
Case Presentation: A 62-year-old woman with a history of diabetes mellitus, hypertension, and hypothyroidism presented with a severe headache which was posterior, waxing and waning in nature, and associated with nausea and vomiting. The headache started suddenly five days earlier and had awoken her from sleep. At that time she had presented to the emergency department where she underwent a CT angiogram of the head and neck that did not reveal any acute process. When she returned home, her symptoms persisted and her husband noticed that she was increasingly lethargic and confused. She denied any similar headaches in the past, fevers, chills, vision changes, or recent trauma. On admission, her vitals were notable for a temperature of 35.8 °C, blood pressure of 143/84 mmHg, and heart rate of 124 bpm. Physical exam was significant for intermittent lethargy without nuchal rigidity, skin rashes, or focal neurologic deficits. CT brain imaging showed no abnormalities. Labs were significant for WBC 11.3 x 10^9/L, Na+ 125, fibrinogen 802 mg/dL, CRP 339.2 mg/dL, and ESR 104 mm/hr. IV antibiotics and antivirals were started for meningitis. A lumbar puncture showed clear colorless cerebrospinal fluid with protein 97 mg/dL, glucose 55 mg/dL, RBC 201 cells/microL, and WBC 31 cells/microL consisting of 46% lymphocytes, 29% neutrophils, 25% monocytes, and 0% blasts with no organisms on gram stain. She then underwent an MRI/MR venography of the brain with gadolinium revealing a 1.9 cm pituitary mass with characteristics of a hemorrhaging macroadenoma, abutting but not compressing the optic chiasm. Further testing showed a low morning serum cortisol of 2.0 mcg/dL and otherwise normal levels of serum LH, FSH, alpha subunit, prolactin, IGF-1, and free and total T4. Hydrocortisone was started for adrenal insufficiency and after further infectious workup, antimicrobial treatment was discontinued. Because of pituitary apoplexy, she was transferred for endoscopic transsphenoidal transnasal resection of the sellar mass. She remained clinically stable and was discharged on physiologic hydrocortisone with resolution of her symptoms.
Discussion: This case represents an atypical manifestation of pituitary macroadenoma and a rare phenomenon of pituitary apoplexy presenting as aseptic meningitis, with CSF studies showing a sterile pleocytosis. This is thought to be caused by leakage of blood or necrotic tissue into the subarachnoid space, resulting in meningeal irritation and a clinical picture of acute meningitis [1,2]. A literature search using the phrases “pituitary apoplexy” and “sterile meningitis” or “aseptic meningitis” yielded only eleven similar cases [2-11]. In view of a lack of hormone hypersecretion, this macroadenoma was a clinically nonfunctioning adenoma. These tumors are usually recognized once they become large enough to cause mass effect, which usually manifests with visual symptoms and less commonly with headache [13]. In the present case, the patient exhibited symptoms of both aseptic meningitis and pituitary hypofunction but did not have visual symptoms. Her symptoms were most likely precipitated by pituitary apoplexy and not mass effect. Risk factors for apoplexy which the patient possessed include systemic hypertension and a non-functioning macroadenoma, which have a higher incidence of apoplexy compared to functional adenomas [14].
Conclusions: Pituitary apoplexy can clinically mimick meningitis and produce pleocytosis on CSF analysis. It should be considered in a patient with headache and signs of meningism.