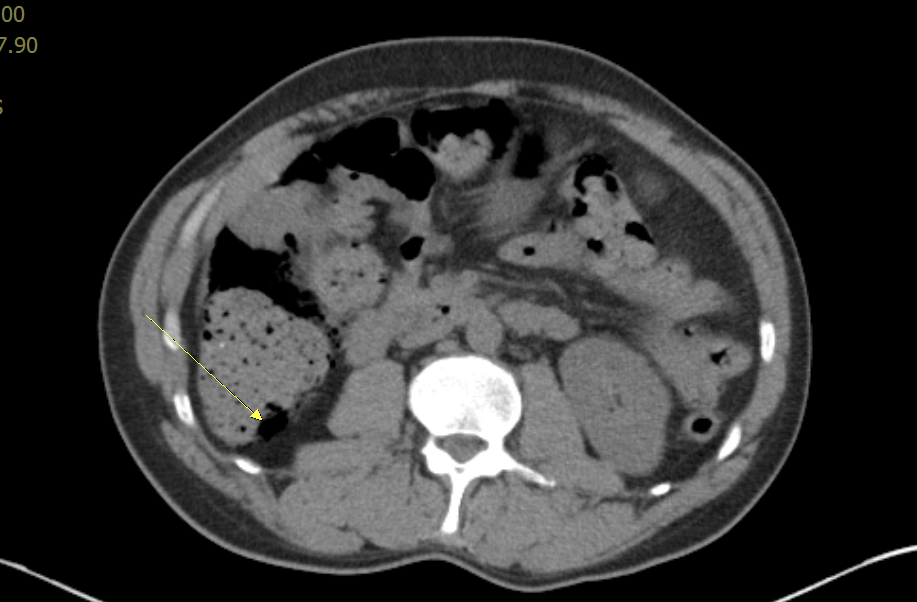
Case Presentation: 50 year old male with past medical history of multiple myeloma status post bone marrow transplant, on tacrilomus presented with 2 day history of worsening abdominal pain, bloating and right-sided flank pain. Physical examination was remarkable for involuntary guarding of the abdomen and absent bowel sounds. CT of the abdomen/pelvis showed pneumatosis involving the right colon, transverse colon, and the stomach. Patient was kept NPO (Nothing By Mouth) and started on broad-spectrum antibiotic and continued on supportive care. Surgical consultation recommended non-surgical management as the patient had no obvious signs of perforation or ischemia. Diet was advanced as tolerated. Patient’s condition improved with conservative management and was discharged home on oral antibiotics ciprofloxacin and metronidazole.
Discussion: Pneumatosis Intestinalis (PI) is the accumulation of gas-filled cysts in the wall of small or large intestine. It is reported that about 15% of cases of PI are idiopathic while 85% of cases are secondary to gastrointestinal illness like inflammatory bowel disease, endoscopic procedures, chronic pulmonary diseases, connective tissue disorders, infections and immunosuppressive state. The etiology is well established and is thought to be multifactorial. Several theories have been proposed and the most widely accepted theory is the mechanical theory. According to this, any condition that disrupts the mucosal integrity and allows the gas to dissect into the intestinal lumen. Bacterial theory proposes that gas forming bacilli enter the submucosa through the mucosa with increased permeability and eventually producing gas within the bowel wall. Lastly, according to the biochemical theory, excessive amount of hydrogen gas is produced by luminal bacteria through fermentation of carbohydrates and the pressure of the gas increases within the intestinal lumen. This forces the gas to dissect through the mucosa and get trapped in submucosa. This theory is supported by the high content of hydrogen gas in the cyst as high as up to 50% and the resolution of the PI with metronidazole.
Conclusions: Pneumatosis Intestinalis is a rare condition characterized by the presence of gas in the bowel wall. Predisposing factors include gastrointestinal illness, pulmonary disease, immunosuppressant agents and many other diseases . In our patient, immunosuppressive therapy was likely the predisposing factor. Immunosuppressive agents overtime can cause the mucosal breakdown and can also cause Peyer’s patches in the bowel to shrink which results in disruption of mucosal integrity and resulting in gas accumulation in the bowel wall. PI can usually be treated conservatively with bowel rest, supportive care and broad spectrum antibiotics if no signs of peritonitis, ischemia or perforation are present.