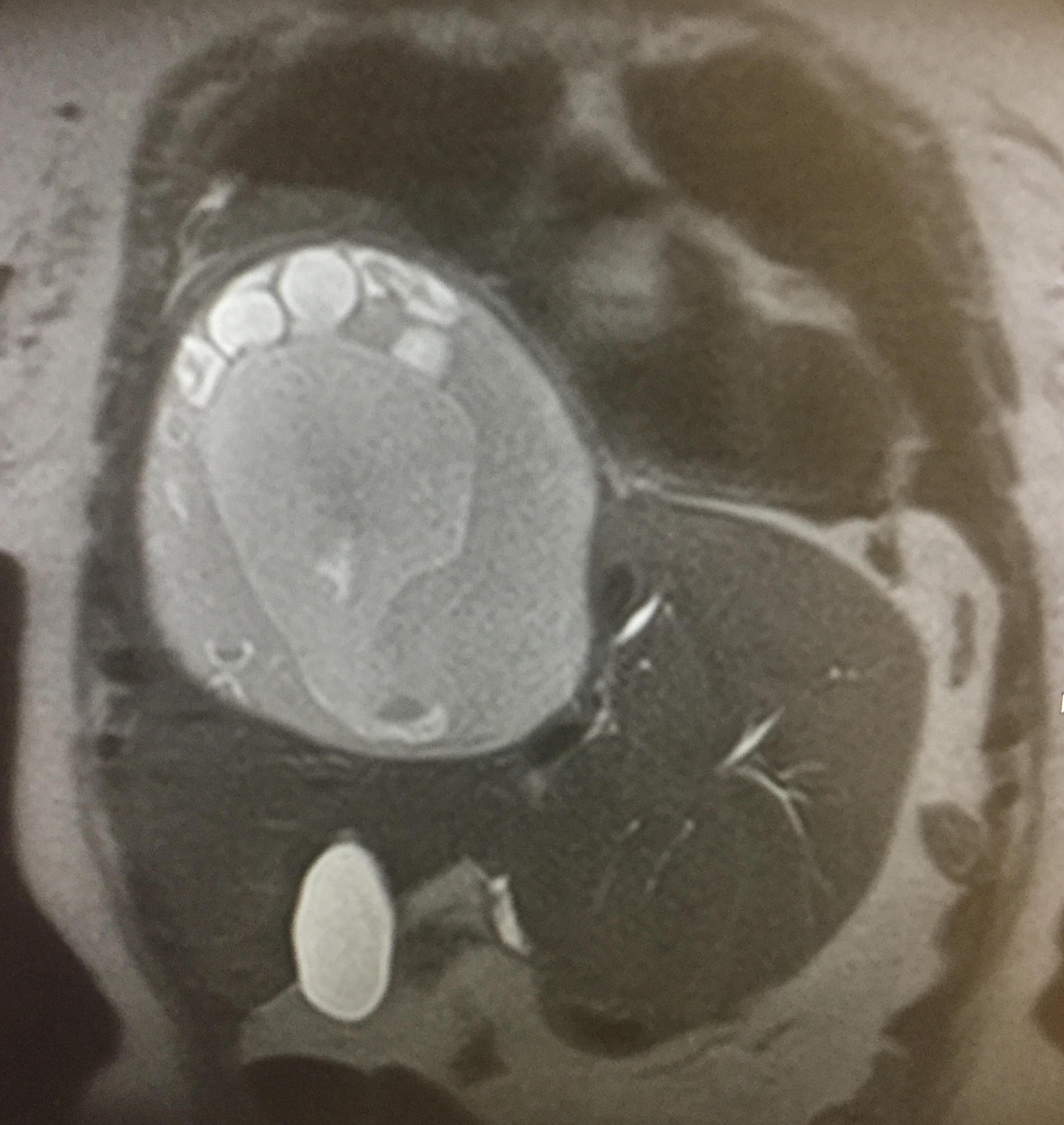
Case Presentation: 74 year old Armenian female with no past medical history presented to the ED twice for community acquired pneumonia, with a right lower lung infiltrate/atelectasis on chest x-ray. Serology labs include WBC 11 with 25% bands, ALP 141 and conjugated bilirubin 0.7. Upon her third visit, she began to have persistent fevers and chills with nausea and vomiting of bilious material. MRI showed elevation of the right hemidiaphragm secondary to a 13cm x 18cm right lobe liver cyst encapsulating multiple cysts and right middle lung atelectasis with multiple foci of air consistent with abscess formation. Echinococcus granulosus workup was positive. She was treated with albendazole for 2 weeks prior to undergoing aspiration and resection of the cyst of up to 2 liters, and partial liver resection. A possible biliary source of her sepsis was investigated by a DISIDA scan, which showed a hepatobiliary-right lower lobe bronchial fistulous communication and a stent was inserted via ERCP.
Discussion: Hydatid disease is a parasitic infestation by a tapeworm of the genus Echinococcus, involving 3 out of 4 species relevant to the human body. Morbidity is typically secondary to cystic rupture or infection, biliary/bronchial obstruction, cirrhosis or hydrocephalus. Due to the known extrahepatic effects of hydatidosis, it is important to consider alternative diagnoses in high risk patients, as shown in this patient who had been misdiagnosed twice with pneumonia. It was not until later that her symptoms were established as being secondary to mass effect and fistula formation. Spillage occurs in 2-25% of cases with an operative mortality rate of 0.5-4%, primarily from anaphylaxis. Several criteria must thus be met in order for patients to be treated appropriately in the hospital; otherwise transfer to a capable facility is warranted. This includes experienced surgeons, ID consultants, radiologists, availability of scolicidal agents and a well-equipped ICU. A rare postoperative complication is a biliary fistula secondary to sudden intracystic decompression, as demonstrated in this patient.
Conclusions: Polycystic hydatid liver disease is rare in Northern US, with a prevalence of <1 case per 1 million inhabitants. The marked increase in immigration and transcontinental transportation have caused an increase in prevalence, leading to the necessity for physicians to be more aware of its diagnosis, management and complications. Perioperative prophylaxis with benzimidazoles is warranted in patients with cystobiliary fistula or infected cysts and is continued 1 month after intervention, although exact duration of treatment has not yet been established.