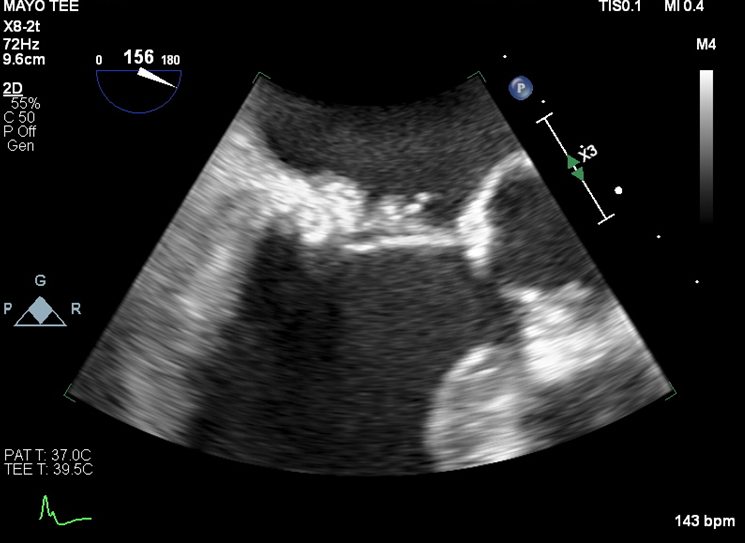
Case Presentation: An 82-year-old female with past medical history of paroxysmal atrial fibrillation, hypertension, CKD stage 3, and recurrent Pseudomonas aeruginosa urinary tract infection was admitted to a cardiology inpatient service for generalized weakness and atrial fibrillation with rapid ventricular response.Her recurrent UTIs had been occurring monthly for the past year. She was noted to have non-obstructive nephrolithiasis and recent ureteroscopic stone extraction was attempted but unsuccessful. A previously placed ureteral stent was retrieved. Her cardiac history was significant for a recent TEE-guided cardioversion a week prior to admission. At that time, moderate mitral valve calcification was noted, but there was no thrombus or vegetation. She was continued on her therapeutic apixaban.On admission, she was afebrile, and noted to have mild tenderness on palpation over the left flank region. Outside hospital blood cultures were positive for P. aeruginosa, and patient was started on cefepime for presumed pyelonephritis and bacteremia. On day two of hospitalization, the patient had an acute right MCA embolic stroke with multiple other tiny embolic infarcts. Work up included a TEE which showed exuberant amount of posterior mitral annular calcification with 1 cm mobile component, with differential including caseous degeneration, thrombus, or vegetation. CT abdomen and pelvis showed evidence of multiple splenic infarcts.Diagnosis of infective endocarditis (IE) was suspected on repeat TEE three days later, when the mobile mass was re-visualized at a significantly greater size of 2 cm with a multi-lobulated heterogeneous appearance. The patient was switched to ceftazidime with extended infusion and underwent replacement of mitral valve in the subsequent week. Gentamicin combination therapy was considered but was not possible due to resistance. In the setting of progressive mitral regurgitation due to P. aeruginosa IE, the patient underwent mitral valve replacement, with valve cultures growing P. aeruginosa.
Discussion: IE caused by P. aeruginosa is uncommon, and when it does occur, is often associated with IV drug use involving the tricuspid valve, or hardware such as prosthetic heart valves or pacemakers. This patient had recurrent UTI with potential repeated blood stream exposure. Cases of IE involving mitral annulus calcification (MAC) have been reported, but no epidemiologic analysis has been performed to identify MAC as a risk factor for infective endocarditis. MAC may obscure visualization of potential abscess or vegetation.Treatment of P. aeruginosa IE usually requires both antibiotic and surgical interventions. The use of two pseudomonal agents should be considered.
Conclusions: While rare, P. aeruginosa endocarditis can occur in non-IV drug users and should be considered in a patient with recurrent bacteremia and weeks history of generalized weakness. Management of Pseudomonas endocarditis should include infectious disease consultation, use of dual-antibiotics, and strong consideration for valve replacement surgery.