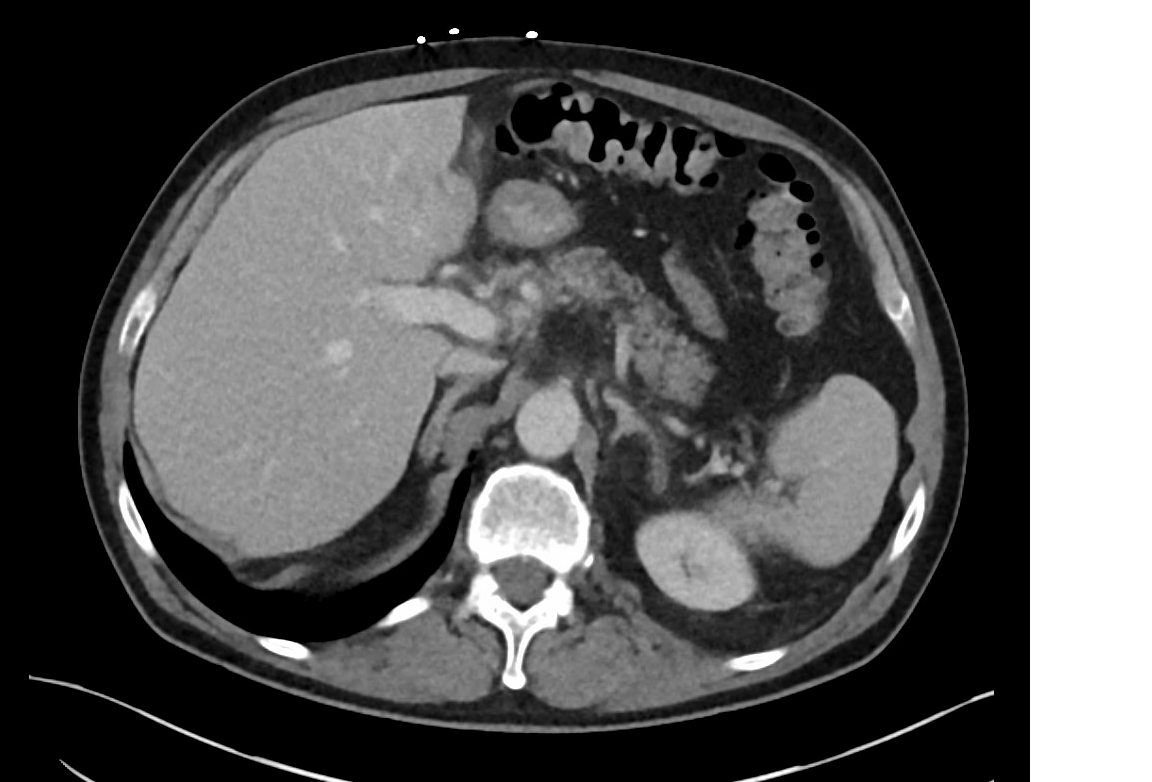
Case Presentation: A 70-year-old male presented to ED with a 10-day history of fever with chills, sweating, abdominal pain and generalized weakness. The abdominal pain was predominant in right lower quadrant (RLQ), accompanied by nausea, vomiting, loss of appetite and significant weight loss more than 10 lbs. in 10 days. He denies jaundice, pruritus, constipation, hematochezia, melena, clay colored stool, acid reflux, dysphagia, odynophagia, GU symptoms, any recent travel or sick contact.On clinical examination, general condition: ill looking.pulse: 101 bpm BP 142/87 mmhg, RR 20, patient temperature 100.6°F, mild abdominal tenderness localized in RUQ and RLQ without distension. His initial lab work showed leukocytosis 20,000, elevated ESR, elevated CRP and hyponatremia. Mildly deranged liver function tests (LFT) with cholestasis pattern and normal bilirubin. Keeping the past history of Provoked PE in mind, CT abdomen/pelvis with iv contrast was done, which showed Left portal vein thrombosis suggestive of thrombophlebitis and left colon diverticulosis but without diverticulitis. The patient was started on Meropenem and Levonox, On the 3rd day of admission, blood cultures grew Beta Hemolytic Group C streptococcus in both aerobic and anaerobic bottles, Infective Endocarditis couldn’t be ruled out, so, Transthoracic Echocardiogram was done, showed no vegetation. The patient’s remained Hemodynamically stable with resolution of fever and leukocytosis. Consequently, the patient was discharged home with a six-week course of oral Moxifloxacin, and anticoagulation was discontinued before discharge.
Discussion: Pylephlebitis, also known as suppurative thrombophlebitis, is a rare condition arising as a complication of intra-abdominal infections drained by the portal venous system, often associated with diverticulitis or appendicitis. It is caused by a single pathogen in 94 (42.8%) cases and polymicrobial in 60 (27.2%) cases, which includes Escherichia coli (25%), Bacteroides spp(17%), and Streptococcus spp. (15%), non-identifiable pathogen in 30% [3]. The common presenting symptom was fatigue (95%), fever (86%) and abdominal pain (82%). laboratory findings were leukocytosis (80%), elevated liver enzymes (69%), hyperbilirubinemia (55%), and anemia (55%). The demonstration of thrombus in the portal vein is the central finding leading to a pylephlebitis diagnosis. CT scan should be preferred over abdominal ultrasound because of its higher definition and the additional investigative ability to identify possible abdominal or pelvic infective foci (10). Complications of pylephlebitis include thrombus propagation, hepatic abscess, hepatic and splenic infarctions, and chronic thrombosis (12) and mortality rates range from 8.7% -19 % (10). Combination of anticoagulants and antibiotics is the mainstay of therapy. However, anticoagulation remains controversial since successful resolution of pylephlebitis has been reported with or without anticoagulation (8)
Conclusions: Pylephlebitis is a rare, yet severe condition acquired secondary to intra-abdominal or pelvic infections of the organs drained by portal venous circulation with multiple etiological factors. Its occurrence with Group c streptococcus is an unusual occurrence. Contrast enhanced CT is the preferred diagnostic modality and antibiotics is the mainstay of treatment.