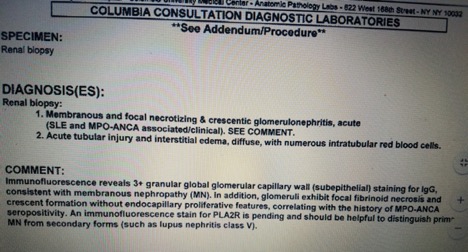
Case Presentation: 51-year-old Hispanic male with past medical history significant for SLE treated with Plaquenil for the past four years and Idiopathic thrombocytopenia (ITP) requiring splenectomy presented with one-week history of hematuria and worsening bilateral flank and abdominal pain. Physical examination revealed petechiae on bilateral lower extremities and edema. Laboratory data was significant for a creatinine of 10.9, with a previous creatinine level of 0.8 two months prior along with urinalysis significant for hematuria and proteinuria. Patient received pulse dose steroids for presumed rapidly progressive glomerulonephritis secondary to SLE. He was initiated on hemodialysis. Further autoimmune work up revealed positive ANA (1:1280), P ANCA and Myeloperoxidase (MPO). Kidney biopsy showed focal necrotizing and crescentic pauci-immune glomerulonephritis suggesting AAV superimposed on a background of membranous nephropathy. He received plasmapheresis for in addition to Rituximab for ANCA associated RPGN. He was continued on oral prednisone. Patient’s symptoms improved during hospital course. Creatinine improved to 1.6 and hemodialysis was stopped about six weeks after discharge.
Discussion: Typically, SLE and AAV are two separate clinical entities and rarely have been found to occur simultaneously. However, few cases of SLE /AAV overlap syndrome have been observed on renal biopsies with patterns consistent with lupus nephritis and AAV. SLE/AAV overlap syndrome carries features of both diseases, which includes skin nodules, arthritis, serositis, cytopenia, malar eruption and pulmonary hemorrhage. One of the most frequent presentations involved in this syndrome is RPGN as seen in our patient proven by kidney biopsy exhibiting features of SLE and ANCA associated vasculitis. Our patient’s age, positive ANA, anti-MPO antibodies and histopathological renal disease were typical for SLE/AAV syndrome however it is more commonly seen in females. The exact pathophysiology is unknown but one theory suggests that SLE/AAVE overlap syndrome may be a part of global poly autoimmunity as our patient also had ITP. Another theory suggests that neutrophil activation that is seen in AAV and SLE may be the precipitating factor in the pathogenesis of this syndrome. In order to understand the exact pathological mechanism of this rare devastating disease and further treatment options, we need more documentation and research of SLE/AAV overlap syndrome.
Conclusions: Few cases of Systemic lupus Erythematous (SLE) and ANCA associated vasculitis (AAV) overlap syndrome have been reported in literature. This syndrome is characterized by rapidly progressive glomerulonephritis, arthritis, pulmonary hemorrhage, both ANA and MPO antibodies. Majority of the cases occur in women, but our case is unique because we had a male patient with SLE/AAV syndrome presenting only with renal involvement. Due to limited documentation of this syndrome in literature, it is crucial to identify this entity and treat appropriately. It becomes clinically challenging as both diseases share many clinical symptoms. Further studies are required to investigate the shared pathogenesis of SLE and AAV and their co-occurrence as a syndrome in order to accomplish targeted therapy.