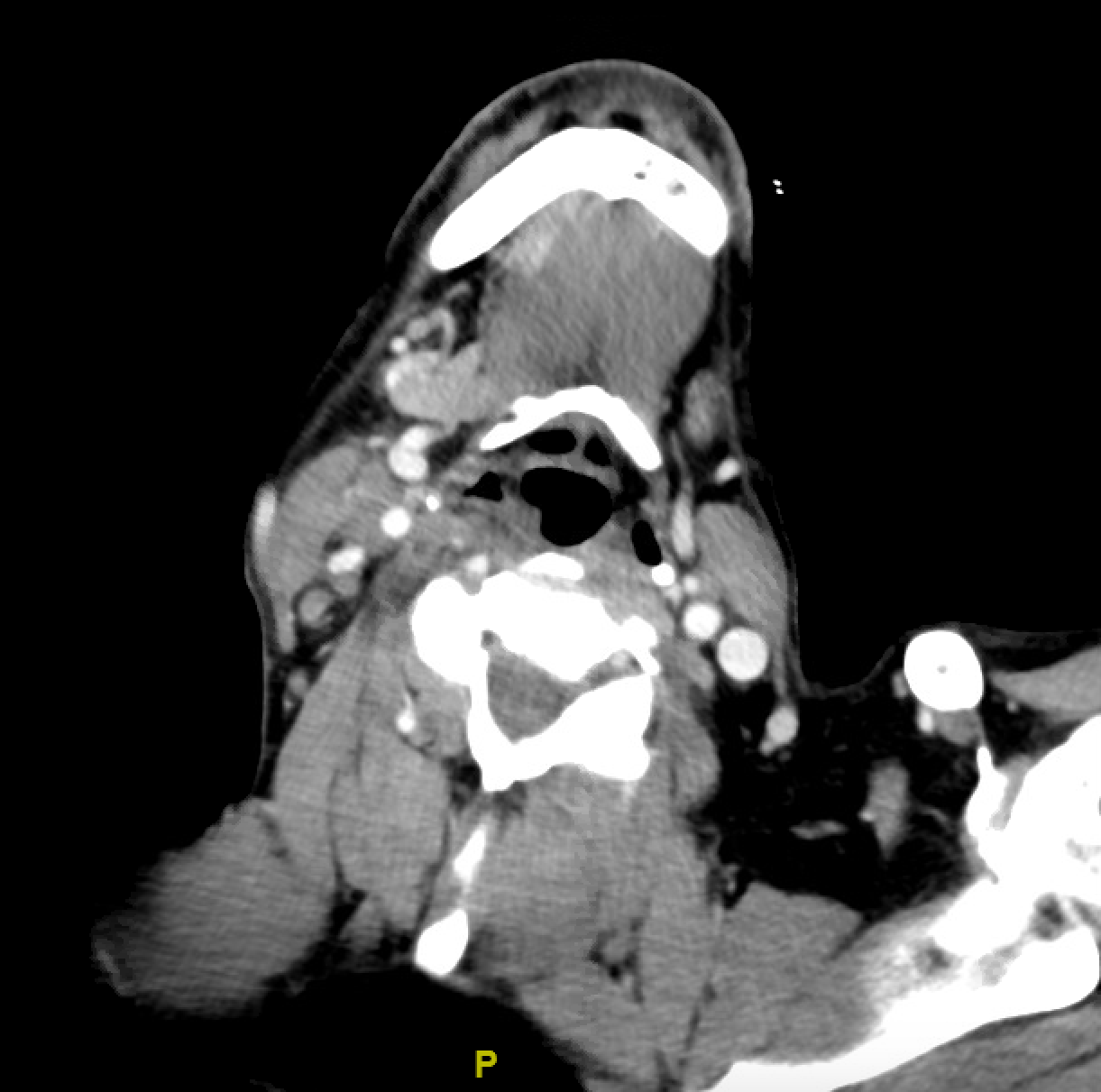
Case Presentation: A 58-year-old male patient was brought by EMS after he was found to have an episode of syncope preceded by nausea, vomiting, dizziness while he was on his way to the supermarket. His past history was significant for hypertension, end stage kidney disease on chronic hemodialysis, and a recent diagnosis of stage IV squamous cell carcinoma of the Rt tonsil (with right jugular chain lymphadenopathy). He had undergone a prophylactic L sided tonsillectomy a week prior to admission. The patient was found to have a HR of 30s with BP in 80s/40s. EKG showed junctional bradycardia with HR in the lower 40s which immediately resolved after 0.5 mg atropine and IV fluid administration.Hospital course was notable for an episode of dizziness with telemetry showing sinus bradycardia with HR in 30s, which was accompanied by hypotension with systolic BP in the 60s. The patient was transferred to the Cardiac Care Unit for closer heart rhythm monitoring. An electrophysiology (EP) study was performed which was negative for SA-AV nodal or His-Purkinje conduction system disease. An implantable loop recorder was placed with electrophysiology follow-up in two weeks. During his hospital stay, it was noted that the patient would sleep only on one side. When questioned about it, he reported that he would become dizzy if he slept on his right side. This prompted a thorough exam of his neck which revealed enlarged lymph nodes at the base of the right neck. With a negative EP study ruling out intrinsic conduction system disease, recent angiography negative for significant coronary obstruction, and no offending medications, the carotid sinus syndrome (CSS) due to compression of carotid sinus with Rt sided lymph nodes are presumed to be responsible for syncope episodes.
Discussion: With advances in modern medicine, there has been a steady shift of the epicenter of patient care from the bedside to documentation rooms filled with computers. In a study conducted at a major academic medical center, two-thirds of internal medicine residents reported that they spend in excess of 4 hours daily while in the hospital setting on documentation and clerical duties, with only slightly more than a third of residents spending this same amount of time in direct patient care 1.While technology, EMRs and sophisticated diagnostic tests have aided in the overall improvement of patient outcomes, it is essential to keep in mind that their purpose is to supplement a thorough history and physical exam, and not to replace them. In this case, the physical exam missed the extensive cervical lymphadenopathy, and it wasn’t until patient reported feeling dizziness if he lies on the right side that the lymph nodes were examined and the question regarding CSS secondary to lymph node compression was raised. This finding was a reminder of the importance of detailed physical exam which unfortunately sometimes can be missed during daily clinical practice.
Conclusions: Thorough physical examination is an important part of clinical diagnosis, in this case it could have possibly prevented the patient’s subsequent decompensation, and also decreased overall cost to the healthcare system by avoiding unnecessary testing and decreased length of stay. Some measures we suggest bringing the focus of medical education back to the basics include bedside rounding by the medical team, and a greater focus on examination skills training and assessment in medical school.