Case Presentation:
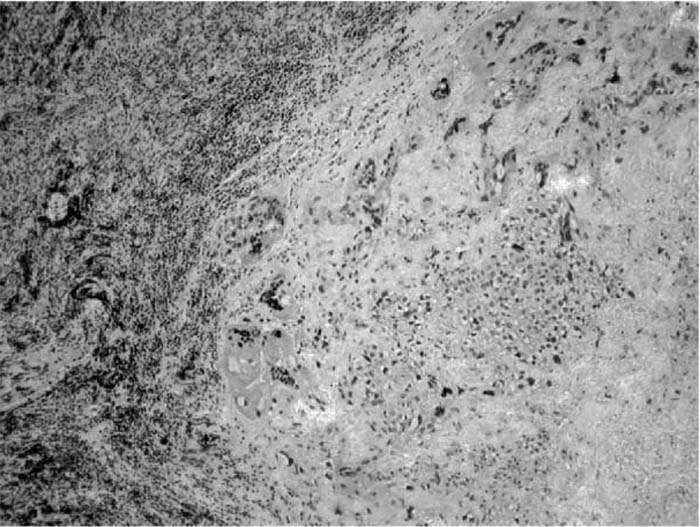
Choriocarcinoma accounts for 1% of testicular carcinomas. Choriocarcinoma primarily spreads hematogeneously into viscera and lungs and involves retroperitoneal lymph nodes and liver. Human chorionic gonadotropin (HCG)‐induced hyperthyroidism in germ‐cell cancers is rare, and only a limited number of reports exist in the literature. Hyperthyroidism resulting from molar pregnancies, hyperemesis gravidarum, and choriocarcinoma is more common in women, but testicular carcinoma‐induced thyrotoxicosis occurs infrequently. This case presentation is an unusual example of hyperthyroidism resulting from testicular choriocarcinoma. A 33‐year‐old man with a history of undescended testes as a child initially presented with constipation and lower abdominal pain for 1 year. He was treated for presumed irritable bowel syndrome, but his symptoms progressed to early satiety and abdominal fullness. He subsequently developed dysphagia, hemoptysis, and left groin pain. A chest X‐ray revealed mediastinal widening. A subsequent computerized tomography scan of the chest revealed a large 7 × 8‐cm mediastinal mass with multiple lymph nodes. Medi‐astinoscopy displayed a large carinal mass, and lymph node biopsy demonstrated high‐grade metastatic choriocarcinoma, Testicular ultrasound revealed a solid mass in the left testicle consistent with testicular neoplasm. He was admitted for chemotherapy and found to have sinus tachycardia. He also reported palpitations, a 16‐pound weight loss, and tremors. Thyroid‐stimulating hormone was 0.02, and free T4 was 2.82. Beta‐HCG levels were greater than 200,000 IU/L. After initiation of chemotherapy and methimazole with propanolol, the patient's symptoms improved.
Discussion:
In a review of the literature about patients with choriocarcinoma and hyperthyroidism, thyroid function returned to normal and HCG concentration decreased after the initiation of chemotherapy . Although secondary hyperthyroidism from metastatic testicular choriocarcinoma is rare and typically subclinical, it can be associated with morbidity. Patients at greatest risk are those with HCG levels greater than 200,000 IU/L. Treatment of metastatic choriocarcinoma‐induced hyperthyroidism is focused on chemotherapy: as cancerous cells are killed, there is a subsequent decline in HCG levels and therefore decreased TSH stimulation. Thionamides and beta‐biockers can be employed for symptomatic relief of hyperthyroidism in conjunction with chemotherapy.
Conclusions:
This case demonstrates the rarity of testicular chorio‐carcinoma‐induced hyperthyroidism and the need for continuous evaluation of paraneopiastic syndromes associated with neoplasms.
Author Disclosure:
A. Khanna, none; R. Bhasin, none: J. Winegarden, none; S. Krishnan, none.