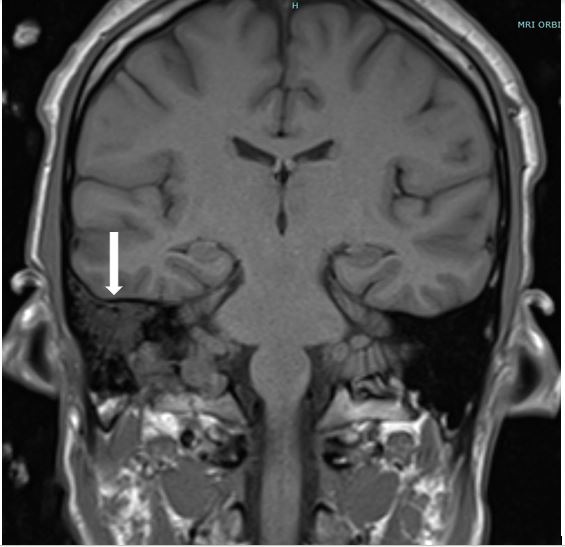
Case Presentation: A 25-year-old African American male presented with complaints of headache and acute painful vision loss in his left eye. He had stable vital signs. On exam, he had 20/20 vision in his right eye with intact visual field and 20/400 vision in his left eye with superior temporo-nasal visual field loss. Fundoscopic exam of the left eye showed diffuse cotton wool spots. Labs were remarkable for elevated CRP of 17.3 and ESR of > 130. CT head revealed no acute hemorrhage, however an MRI of orbits and face revealed a dural venous sinus thrombosis of right transverse and sigmoid sinus extending to the right internal jugular vein. He was started on therapeutic enoxaparin.
He had a lumbar puncture with normal opening pressure and normal WBC, RBC, glucose and protein. CSF fluid tests for viral infections were negative. Due to concern of posterior uveitis and disc edema without signs of endophthalmitis, he was started on atropine and prednisolone eye drops.
Later on, he reported a history of painful recurrent oral ulcers and peritonsillar abscess formation. Also, several papules were noticed on exam in the patient’s forearm and hand where he had labs drawn several days ago. Given these discoveries in the setting of his elevated inflammatory markers and bilateral posterior uveitis, there was concern of vasculitis. Work-up with ANCA, ANA, rheumatoid factor, HLA B27, complement levels were normal.
Given his history of painful oral ulcers, posterior uveitis, sinus thrombus, and pathergy, the patient was diagnosed with Behçet’s disease (BD). He was started on 1 mg/kg oral prednisone upon discharge and azathioprine as outpatient.
Discussion: BD is a multisystem vasculitis with a unique geographic distribution. It affects people mostly from eastern Asia to the Mediterranean. Clinical manifestations are classic for relapsing anterior/posterior uveitis, painful recurrent oral and genital lesions.
Criteria for diagnosis is a point-based system using the International Study Group. 2 points each are given to patients with ocular lesions (uveitis), genital apthosis, or oral apthosis. 1 point each is given to patients with skin lesions (papulopustular lesions, erythema nodosum), neurological manifestations, vascular manifestations (thrombosis, aneurysm), or a positive pathergy test. More than 4 points is diagnostic, and our patient had 6 points (ocular, neurologic, oral, pathergy).
Neurologic lesions are rare manifestations of BD. There are only a few reports of first presentation of BD with dural sinus thrombosis. However, their identification has increased due to the increased use of MRI imaging.
Conclusions: This case emphasizes recognizing the neurologic and ophthalmologic manifestations of BD. In addition, BD can present in non-typical ethnic populations, especially in young African Americans. Also, a thorough review of systems may be helpful to identify the associated symptoms in BD patients such as ulcers, skin manifestations, and pathergy that may not initially be found in the presenting history.