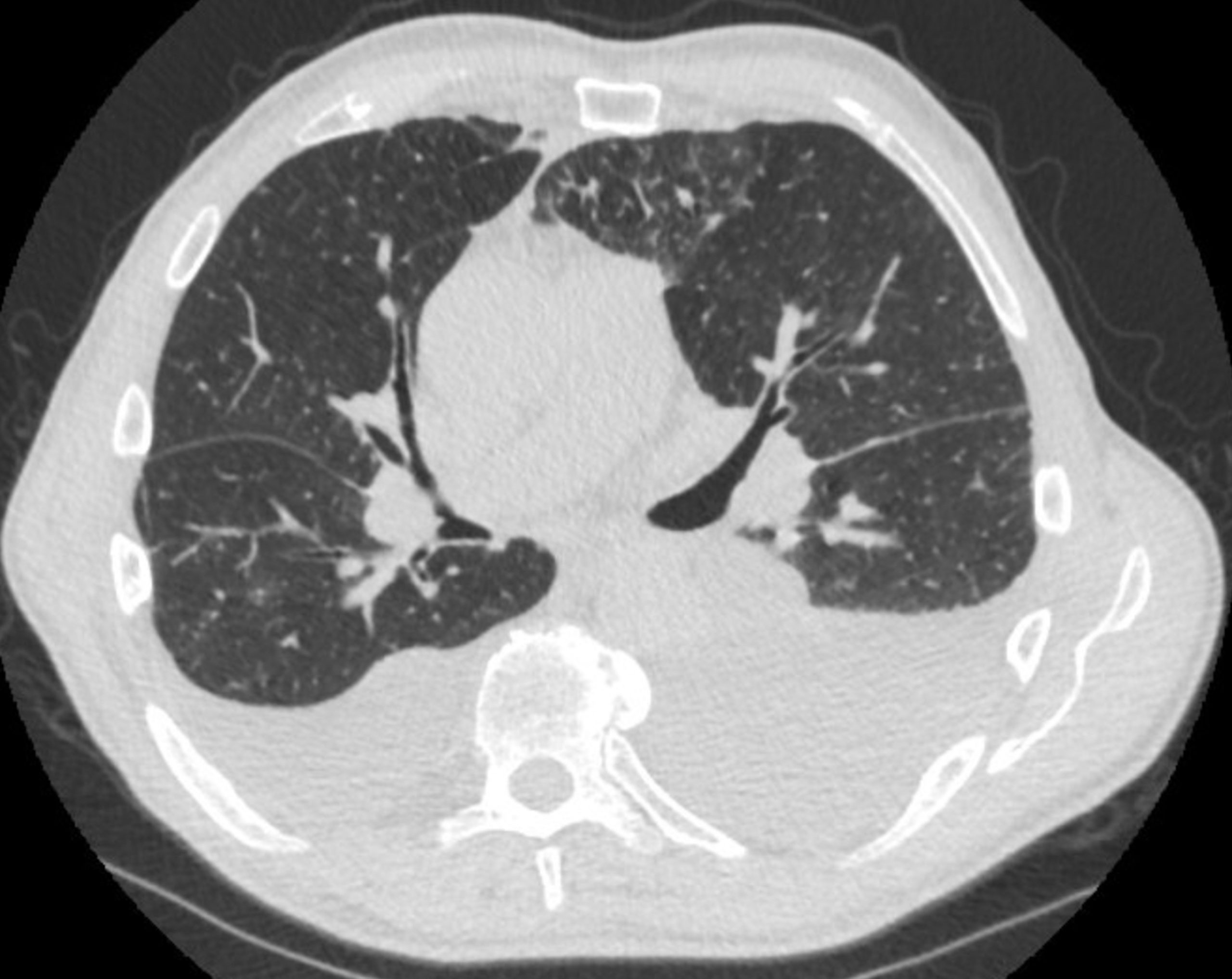
Case Presentation: A man in his 70s with history of benign prostate hypertrophy, diverticulosis, and polymyalgia rheumatica with previously elevated RF and anti-CCP serologies who first developed sinus symptoms and recurrent pneumonias four years prior to his current presentation. At that time, he had CT chest imaging demonstrate bronchiectasis and spirometry reveal an obstructive ventilatory defect. He was also noted to have yellow nails in his hands and feet with unclear etiology. He was started on an airway clearance regimen with occasional bronchiectasis flares over the years that required antibiotics. Prior to this hospitalization, the patient developed worsening shortness of breath and on CT imaging was found to have bilateral pleural effusions. He had an outpatient left sided thoracentesis that revealed a lymphocytic predominant exudative pleural effusion without evidence of malignancy. During this period of close laboratory monitoring, he developed a progressive neutropenia for which he was referred to the ED for additional workup. In the ED, he endorsed weeks of lethargy, a 10-pound unintentional weight loss due to decreased appetite, progressive dyspnea that improved after thoracentesis, worsening lower extremity edema, and generalized weakness. He had no sick contacts, fevers, infectious symptoms, cardiac complaints, or new rash. He was COVID vaccinated and boosted. Family and social history were non-contributory to the patient’s presentation. Vital signs were normal. On exam, he was noted to have yellowing and clubbing of his nails in all four extremities as well as right greater than left lower extremity edema.
Discussion: The patient had extensive testing performed during his hospitalization but was ultimately diagnosed with Yellow Nail Syndrome which is is an uncommon syndrome with less than 400 cases reported in the literature. The pathophysiology is thought to be secondary to lymphatic fluid accumulation throughout the body leading to the triad of yellow nails, recurrent sinopulmonary infections with bronchiectasis and pleural effusions, and lower extremity edema. This triad of symptoms is often not present simultaneously making the diagnosis even more difficult to make. Treatment is focused on addressing the symptoms created by the various manifestations of the disease. As such, vitamin E or clarithromycin is often used to treat the nails, sinus and airway clearance regimens, antibiotics, and pleural drainage are used to treat the sinopulmonary components, and compression stockings and diuretics are used to manage lymphedema. Although there have been numerous proposals that Yellow Nail Syndrome is associated with an underlying malignancy or autoimmune process, a clear underlying inflammatory driver is only seen in a minority of cases. Median survival in a cohort of 41 patients with Yellow Nail Syndrome was 132 months which was substantially lower than a control population.
Conclusions: For the practicing clinician, Yellow Nail Syndrome is a diagnosis that should be entertained when a patient, most commonly in their fifth through seventh decade of life, presents with recurrent sinopulmonary complaints in the setting of lower extremity edema or nail changes. Greater appreciation and earlier diagnosis may ultimately allow patients to get the subspecialist care needed to appropriately manage their symptoms.