Case Presentation: A 76-year-old female with Diabetes Mellitus and COPD on 3L home oxygen and chronic prednisone, presented to the Emergency Department with diffuse abdominal pain and nausea. She denied alcohol or tobacco use. On arrival, vital signs were significant for tachycardia with new oxygen requirements. Physical exam was notable for epigastric, left lower quadrant, and suprapubic tenderness. Laboratory studies revealed leukocytosis of 15,200 mm3, glucose of 403 mg/dL, lipase greater than 3000 U/L, serum calcium of 9.8 mg/dL, alkaline phosphatase of 62 U/L, aspartate aminotransferase of 12 U/L, alanine aminotransferase of 17 U/L, triglycerides of 245 mg/dL, and IgG-4 of 6 mg/dL. Abdominal ultrasound revealed cholelithiasis without biliary dilatation. Computed tomography (CT) of her abdomen revealed new prominent inflammation of the pancreatic head and adjacent duodenum, and the pancreatic duct borderline enlarged at the body measuring 4-5 mm. An infectious workup was unremarkable. Medication reconciliation, after work-up, revealed recent initiation of TMP-SMX three weeks prior for prophylaxis while on chronic prednisone for COPD. For treatment, she received intravenous fluids, a pain regimen, and a proton pump inhibitor. TMP-SMX was switched for Atovaquone for continued prophylaxis. Her abdominal pain gradually subsided. A repeat CT of her abdomen showed improvement of her pancreatitis. She was subsequently discharge home with outpatient follow-up.
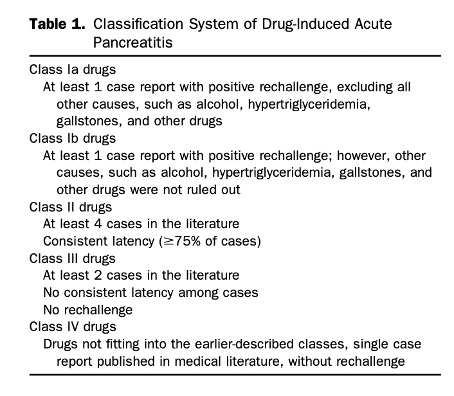
Discussion: Drug-induced acute pancreatitis (AP) is responsible for 0.1%-2% of AP incidents, with mortality rates for severe pancreatitis reaching as high as 30%. Drug-induced AP is often overlooked as the diagnosis is based on exclusion with workup largely dependent on eliminating concomitant factors of pancreatic injury. The Badalov classification system of Drug-induced AP (Table 1) offers a guideline for classifying drugs based on the number of published cases, rechallenge, and latency. Within this system, TMP-SMX is traditionally in Class 1b. It is important to re-evaluate where drugs fit into the classification system, and recent cases have demonstrated a rechallenge of TMP-SMX causing pancreatitis. We were not able to rechallenge because of the risk associated with medication exposure. Our case is unique in that it demonstrates a definite relationship between acute pancreatitis and TMP-SMX in a patient who recently started the antibiotic.
Conclusions: We present this case to increase awareness of acute pancreatitis with TMP-SMX, as it is a widely used first-line antimicrobial agent for Pneumocystis jirovecci pneumonia prophylaxis, and to emphasize the importance of medication reconciliation when exploring the differential causes of pancreatitis.