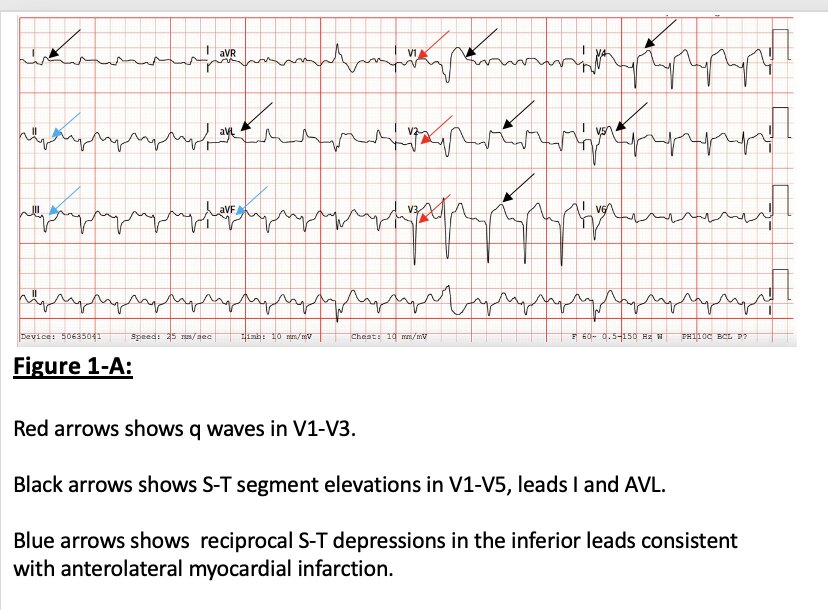
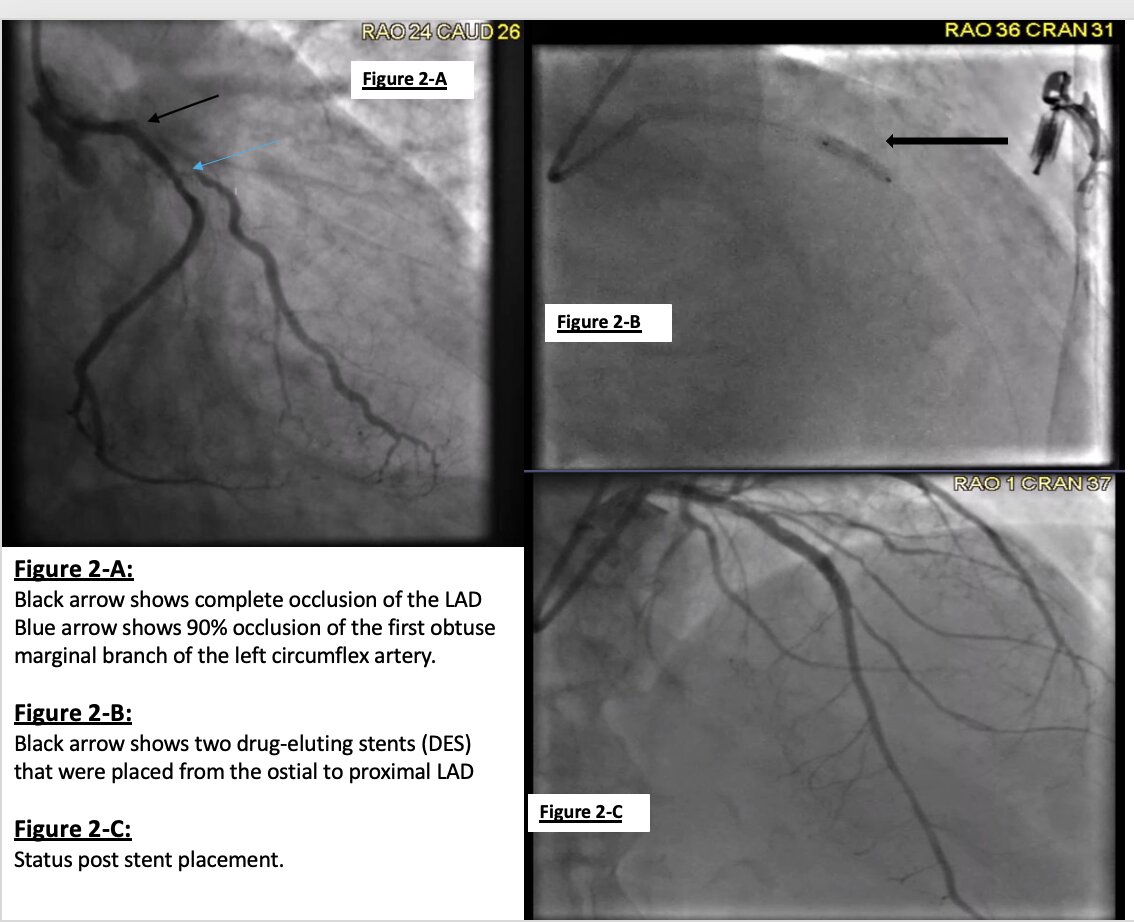
Case Presentation: Pharyngeal pain is typically associated with upper respiratory tract pathology; rarely is it considered the initial presentation of acute coronary syndrome (ACS). Delayed diagnosis and treatment of ACS in such cases can lead to poor patient outcomes and increased mortality (1). A 76-year-old male with a medical history of benign prostate hyperplasia and ulcerative colitis came to the emergency department with a tight, painful throat sensation that lasted five days. He was taking omeprazole because he thought it was due to gastroesophageal reflux disease. He had no known family history of cardiovascular diseases, and he never smoked cigarettes. On examination, he had tachycardia up to 130 beats per minute, but the remainder of the exam was unremarkable. His laboratory values showed an initial troponin of 2.92 ng/ml, which then peaked at 80 ng/ml. The electrocardiogram showed q waves in V1-V3 and S-T segment elevations in V1-V5, leads I and AVL, with reciprocal S-T depressions in the inferior leads, as shown in figure 1-A. A coronary angiogram revealed complete occlusion of the ostial segment of the left anterior descending (LAD) artery (black arrow), as well as 90% occlusion of the first obtuse marginal branch of the left circumflex artery (blue arrow). The findings are shown in Figure 2-A.Two drug-eluting stents (DES) were placed from the ostial to proximal LAD segments with excellent angiographic results, as shown in figures 2-B and 2-C. His procedure was complicated by hemodynamic instability, requiring the placement of an intra-aortic balloon pump (IABP) prior to transfer to the cardiac intensive care unit (CICU) for post-MI care. After IABP removal, he underwent staged percutaneous coronary intervention (PCI) of the obtuse marginal branch, which included balloon angioplasty and the placement of one drug-eluting stent. A post-myocardial infarction echocardiogram showed a left ventricular ejection fraction of 31-35%. He was discharged with guideline-directed treatment for heart failure with reduced ejection fraction, high-dose statins, and dual anti-platelet therapy. A wearable cardioverter defibrillator (life vest) was arranged prior to discharge, as well as outpatient cardiology follow-up.
Discussion: Atypical presentations of myocardial infarction can include various symptoms, including epigastric pain, nausea, sore throat, toothache, and otalgia (2, 3). Studies show that pharyngeal pain has been presented as the lone symptom of acute coronary syndrome (3). An observational study carried out by Yanqing et al. showed that about 56% of patients diagnosed with acute coronary syndrome (ACS) were first admitted to the otorhinolaryngology department, and such patients had a high mortality rate (4). Higher mortality could be due to treatment delay, as a majority of patients first visit a general physician for craniofacial symptoms (5). Our patient was also on proton pump inhibitors, attributing the pain to being of gastrointestinal origin. One possible mechanism for pharyngeal pain could be as a result of the shared innervation of the cardiac and pharyngeal muscles by the vagus nerve. However, the rationale as to why some patients present with throat pain alone and not chest pain is unclear.
Conclusions: Our case report highlights the importance of recognizing pharyngeal symptoms as a possible initial presentation of cardiac ischemia. This is critically important, as early ACS workup and diagnosis curtail treatment delay and allow for improved outcomes, including decreased mortality.