Background: Classically, paracentesis and thoracentesis have been performed by interventional radiology (IR) at our institution. Despite the advantages of IR, the high demand for these services can lead to procedural delays, potentially increasing patients’ length of stay (LOS). Retrospective studies of well-established hospitalist medicine procedural services (HMPS) have shown improvements in length of stay.
Methods: The electronic medical record was mined for all patients who underwent paracentesis or thoracentesis at Butterworth and Blodgett hospitals in Grand Rapids, MI, from 4/1/21-5/01/23. Patients from the pre-HMPS arm (IR) were compared with patients from the HMPS arm. Propensity score matching was employed using multiple variables including age, sex, race, medical comorbid conditions (HTN, DMII, heart failure, cirrhosis, etc.), antiplatelet and anticoagulant use, DRG weight, and procedure type using greedy matching method with control/treated ratio of 1:1. Comparative analysis of the LOS as well as time from order placement-to-completion between HMPS and IR was performed using Wilcoxon Rank Sum Test. Multiple regression with backwards selection was used to find associated predictors of length of stay.
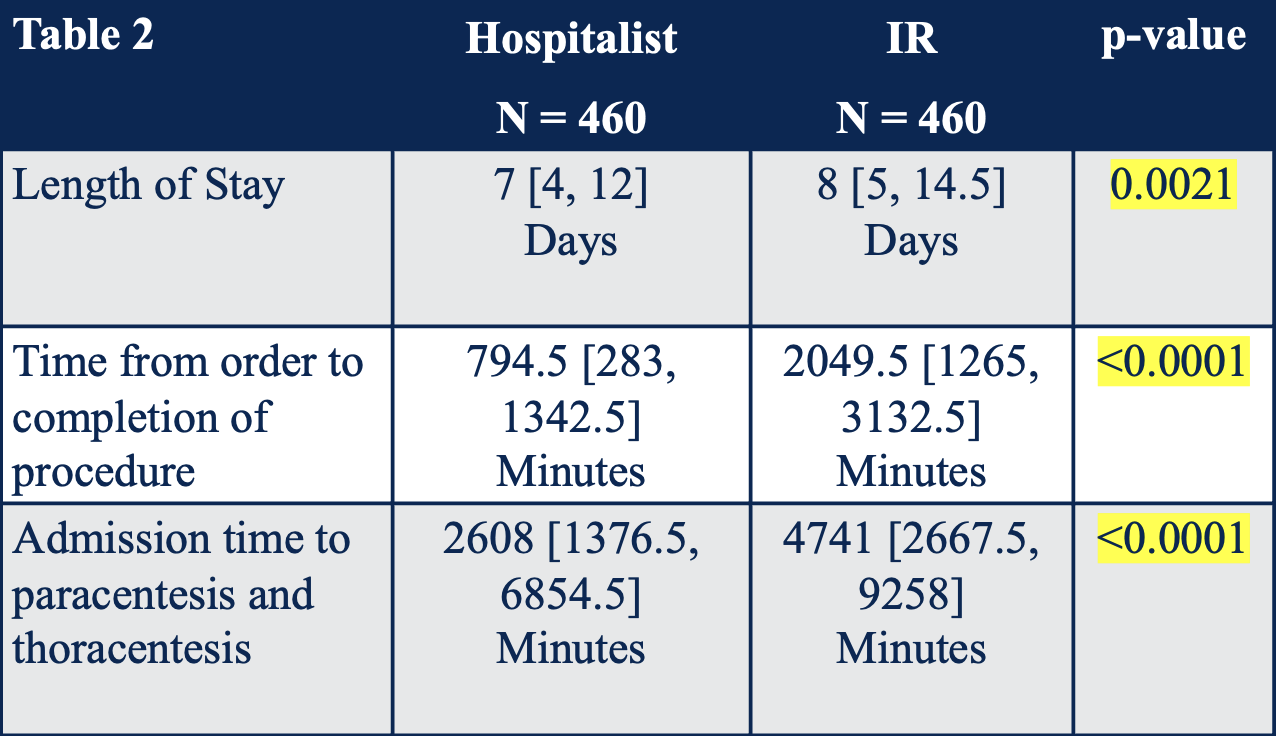
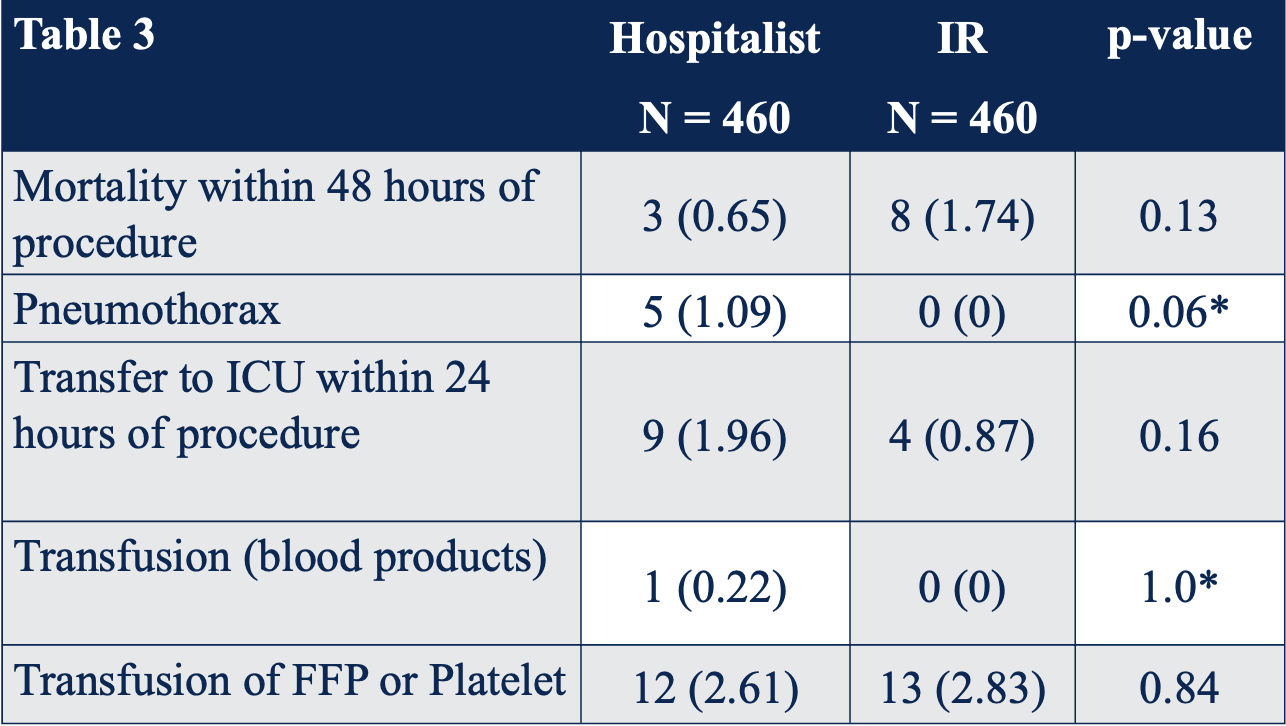
Results: A power analysis determined that a total of 920 patients were required. 50% underwent thoracentesis or paracentesis by IR, while the remaining 50% was performed by the HMPS following its implementation. The propensity-matched group treated by the IR had a median LOS of 8 days compared to 7 days for those treated by HMPS with a p value of .003. Moreover, there was a statistically significant difference in the median time from order to completion of the procedure, 2049.5 minutes for IR compared to 794.5 minutes for HMPS. Complication rates, including mortality within 48 hours, pneumothorax, transfer to ICU within 24 hours, and need for transfusion of blood products were also compared between groups. Although many hospitalists required training, there was no statistically significant difference in overall complication rates between the groups. A higher number of pneumothorax was reported in the HMPS (N=5) compared to IR (N=0), but this was not statistically significant. Time from order-to-completion rather than service was most strongly associated with a decreased LOS and was statistically significant.
Conclusions: Our study has numerous novel components, including evaluating the outcomes during the creation of a new HMPS as well as looking at predictors of length of stay rather than just comparing IR to a HMPS. While the creation of a HMPS did show a significant reduction in LOS, our study shows that time from order to procedure completion appears to be the primary predictor of actual LOS rather than the group performing the procedure. Additionally, the creation of a HMPS can be done with no significant difference in complications.