Background: Coronavirus disease of 2019 (COVID-19) is a novel widespread disease that has a range of manifestation from asymptomatic to fatal. In the United States, there have been approximately 396,000 hospitalizations as of this writing, of which an estimated 25% will require the intensive care unit (ICU)1,2. With the ongoing spread and repeated waves of the disease, it is important to determine practices that may limit COVID-19 patient deterioration that lead to ICU transfers. Our specific aim was to assess patterns of clinical deterioration requiring ICU transfers and identify potential interventions to prevent ICU transfers based on experiences from frontline providers.
Methods: The retrospective descriptive study was completed at an academic tertiary referral center evaluating adult COVID-19 positive inpatients who were admitted to cohort units who required an ICU transfer from 3/21/20 to 5/21/20. Confirmed infection was defined as a positive SARS-CoV2 test during the hospitalization or within 30 days of admission. Data were collected from the electronic health record (EHR) reporting database and through a protocolized chart review. Data collected included admission date and time, transfer date and time to the ICU, transfer date and time out of the ICU, discharge date and time, vitals, respiratory status and reason for ICU transfer as detailed by nursing and physician notes. Reasons for transfer were categorized as respiratory failure, hypotension/hemodynamic instability, electrolyte derangement, neurologic/altered mental status, and other causes. A timeline of important hospital operational, clinical practice guidelines, and EHR modifications for COVID-19 patient management was compiled using email records of those announcements.
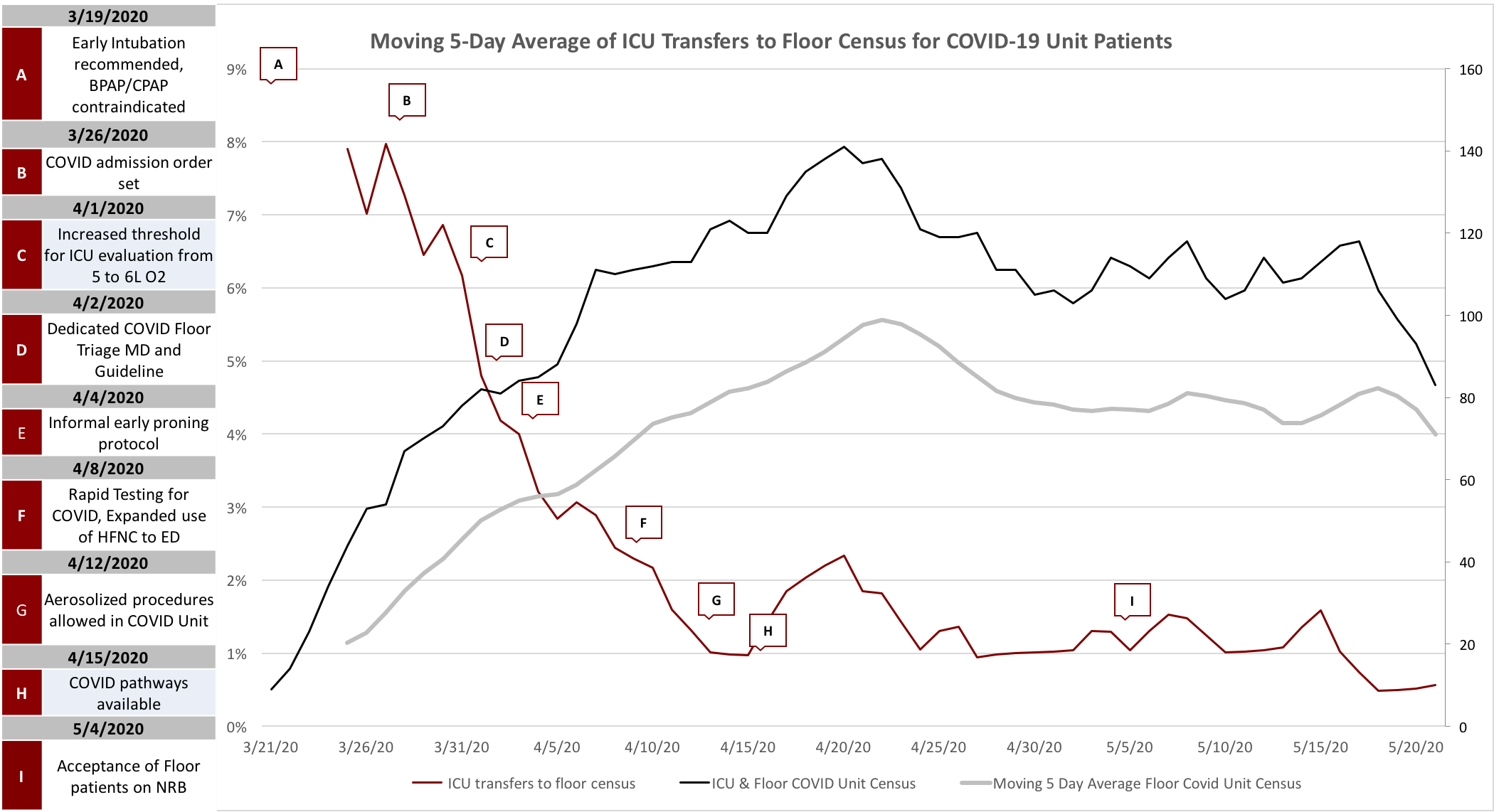
Results: From the opening of the COVID-19 Units on 3/21/20 to 5/21/20 there were 694 total admissions and transfers to the COVID-19 floor unit. Of those, 82 (11%) were unexpected transfers to the ICU. Only 3% of unexpected transfers to the ICU occurred in less than 24 hours of the index floor admission or transfer. The majority (69%) of ICU transfers were due to respiratory failure, neurologic conditions (13%), and hypotension/hemodynamic instability (8%). Respiratory failure was primarily described as increasing oxygen requirement above the floor threshold of 6 L oxygen by nasal cannula. The moving 5-day average percent of ICU transfers over time showed a decrease of ICU transfers over time, with a sharp shift down occurring at the second to third week of the unit opening (Fig. 1). Several clinical care guidelines and pathway interventions were implemented during that period to enhance management of COVID-19 patients and restrict ICU admissions (Fig. 1).
Conclusions: Numerous operational and guideline changes occurred within the first 3 weeks of the COVID-19 unit opening. There was a sharp decline in the percent of ICU transfers in the second to third week. Given the clustering of events, it is hard to delineate the impact of each intervention. However, the rapid implementation of admission order sets, triage guideline, structured treatment pathways did not negatively affect the quality of patient care as measured by unexpected ICU transfers. It may have provided reliable guidance for physicians managing a new disease during an accelerating pandemic and helped reduce unexpected ICU transfers.