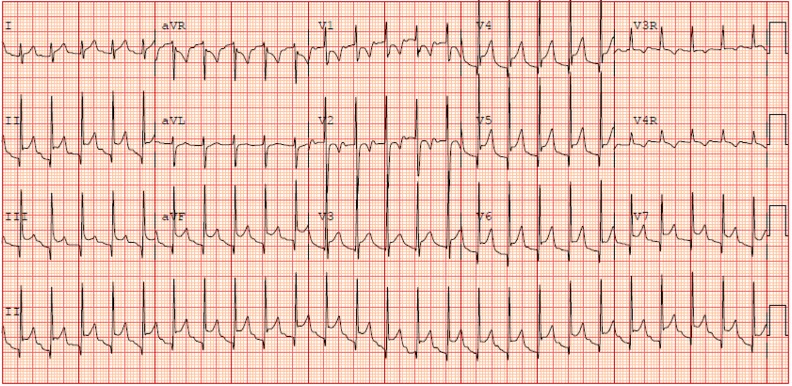
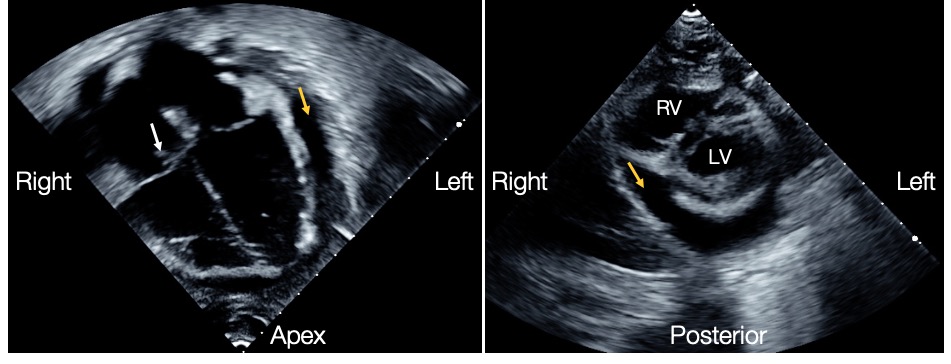
Case Presentation: A previously healthy, immunized 4-year-old female presented with one week of ongoing fevers (Tmax 40oC), left ankle swelling with refusal to bear weight, and right hand swelling and erythema. On presentation, she was febrile (38.9oC), tachycardic (HR 143), hypotensive (BP 60/48), and tachypneic (RR 34). In addition to left ankle and right hand swelling, exam revealed a new gallop with non-displaced PMI, no murmur, strong distal pulses, no hepatosplenomegaly, and lungs clear to auscultation. She was irritable but without altered mental status and was admitted for fluid resuscitation, IV antibiotics, and evaluation of severe sepsis and new cardiac dysfunction. EKG showed diffuse ST elevations and PR depressions concerning for pericarditis (Image 1). Normal troponin was reassuring against myocarditis. Initial echocardiogram revealed a tricuspid valve vegetation, trivial tricuspid insufficiency, and a pericardial effusion that was moderately sized but hemodynamically significant with right atrial wall movement in diastole. Over the next 48 hours, the pericardial effusion increased in size (Image 2), and she demonstrated clinical and echocardiographic signs of tamponade with tachycardia, tachypnea, pulsus paradoxus, and impedance of right atrial filling. Pericardiocentesis and pericardial window were performed. Purulent pericardial fluid was positive for Methicillin Resistant Staphylococcus aureus (MRSA). She was also found to have MRSA bacteremia, bacteriuria, pneumonia, and multifocal musculoskeletal infection with left tibia osteomyelitis, subperiosteal abscess, and pyomyositis, as well as a right metacarpal abscess. The patient responded well to a six-week course of vancomycin and surgical intervention for the musculoskeletal infections.
Discussion: We present a case of disseminated community-acquired (CA) MRSA infection with hematogenous spread to the heart resulting in purulent pericarditis and bacterial endocarditis. Purulent (bacterial) pericarditis is rare, accounting for less than 1% of pericardial disease, and is often associated with concomitant musculoskeletal infection, soft tissue infection, or pneumonia with hematogenous spread to the pericardium. It is potentially fatal and requires prompt recognition, early antibiotic therapy, and procedural intervention. Historically not associated with severe infection, CA-MRSA has a changing virulence pattern and increased incidence of invasive disease. CA-MRSA pericarditis is exceedingly rare in children, with only 6 previously reported cases, and often occurs without risk factors (e.g. immune dysfunction, malignancy, cardiac surgery, pre-existing pericardial disease).
Conclusions: This case highlights that pediatric CA-MRSA pericarditis often occurs in previously healthy, immunocompetent, non-instrumented children. Progression of our patient’s cardiac dysfunction demonstrates the importance of early source control and procedural intervention to decrease mortality. Though rare, purulent pericarditis should be considered in children who present with sepsis and evidence of new cardiac dysfunction.