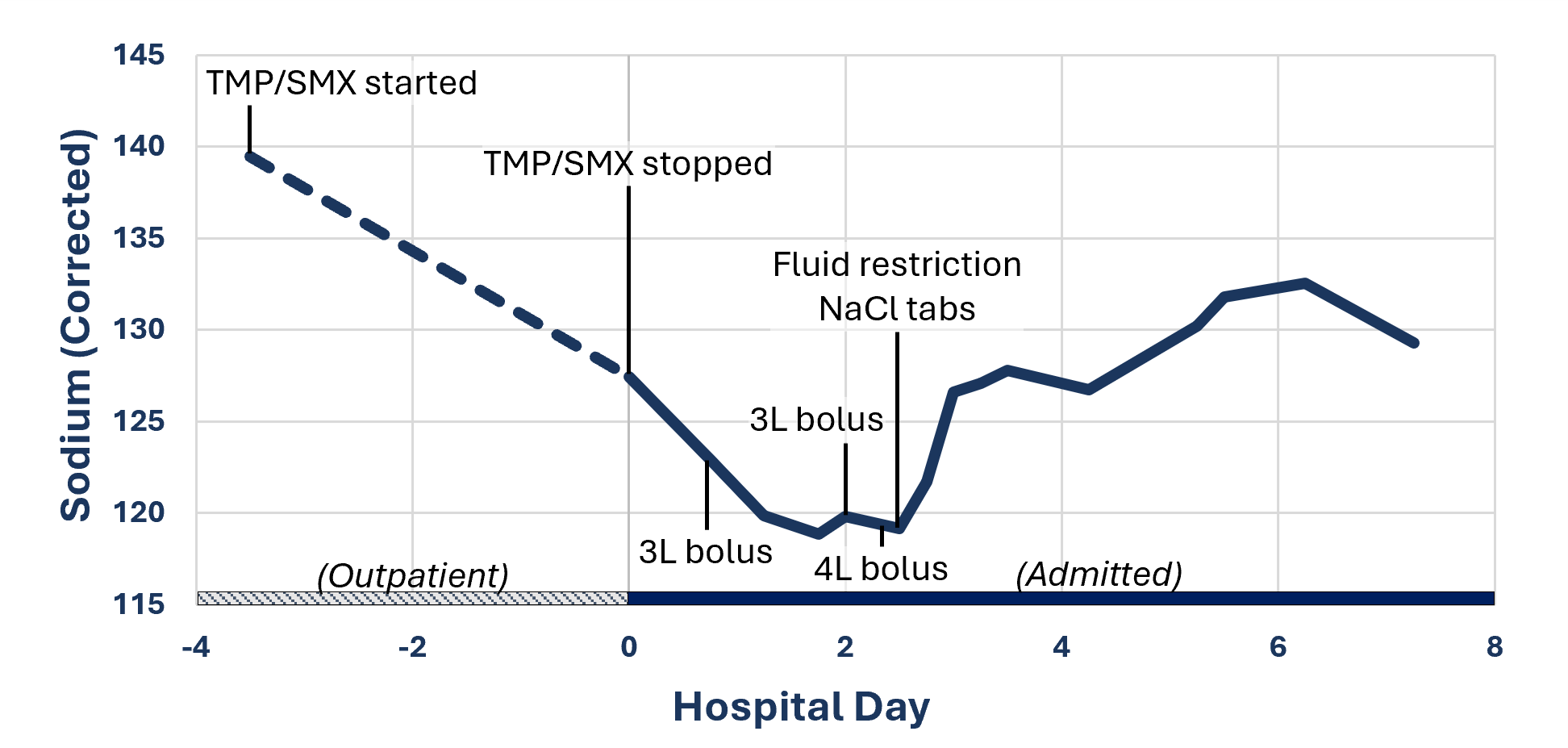
Case Presentation: A 54-year-old woman with type 2 diabetes mellitus with hyperglycemia and hypertension presented to our hospital with new fevers, nausea, vomiting.Four days prior, the patient was found to have a diabetic foot infection and started on trimethoprim/sulfamethoxazole (TMP-SMX) and metronidazole as an outpatient. At this time, her sodium was 133, corrected to 139 for hyperglycemia. The patient then returned with new nausea and vomiting. Initial work up noted temperature of 38.1 °C, WBC 26.2K, sodium of 121, and glucose of 269. Physical exam showed dry mucus membranes and tachycardia. Antibiotics were broadened and TMP-SMX was stopped. She received fluids for sepsis and presumed hypovolemic hyponatremia due to vomiting and was admitted.Studies obtained on hospital day 1 showed sodium of 117, BUN of 42, glucose of 338, serum osmolality of 273 mOsm/kg, and urine sodium 34 mmol/L. Given clinical hypovolemia and persistent tachycardia, she received additional isotonic fluids, with worsening of her hyponatremia. On day 3, she was clinically euvolemic, with labs notable for sodium 118, BUN 15. Fluid resuscitation was held, and she was started on 1g NaCl tabs with a fluid restriction of 1L, with improvement of her sodium. Repeat studies on day 5 of admission showed urine osmolality of 149 mOsm/kg, urine sodium of 28 mmol/L, consistent with a diagnosis of Syndrome of Inappropriate Anti-Diuretic Hormone (SIADH). Her sodium values continued to improve with liberal dietary salt intake and continued fluid restriction. The patient was discharged on day 8 with outpatient follow up.
Discussion: Hospitalized patients may have multiple etiologies of hyponatremia, resulting in equivocal or changing clinical volume assessments. Failure of therapeutic trials to produce the expected effect should prompt reassessment. Our patient was initially evaluated as clinically hypovolemic. However, following fluid boluses, she remained hyponatremic despite improvement in her volume status to euvolemia, at which point she was diagnosed with SIADH. SIADH classically presents with euvolemic hyponatremia, urine sodium >20 and urine osmolality >100. SIADH can present in patients who are clinically hypovolemic for other reasons but cannot be diagnosed until they have been adequately resuscitated to euvolemia per the Bartter and Schwartz diagnostic criteria.TMP-SMX is a very commonly prescribed antibiotic used in inpatient and outpatient regimens. As such, hospitalized patients may be exposed to TMP-SMX in the immediate pre-hospitalization period, as in our case, or be initiated on it during their hospitalization. TMP-SMX is known to cause an increase in serum creatinine and hyperkalemia. A less appreciated side effect is hyponatremia, either due to renal salt wasting or due to SIADH secondary to TMP-SMX. In our patient, with her subsequent labs supportive of a diagnosis of SIADH, a close review of her medication history was performed. Based on previously reported cases, we concluded that her hyponatremia was largely due to TMP-SMX induced SIADH.
Conclusions: This case highlights the importance of reassessing patients with hyponatremia, as there may be multiple reasons for the hyponatremia requiring different treatments. TMP-SMX is a very commonly prescribed antibiotic, and hospitalists should be aware of SIADH as a potential side effect in patients who develop hyponatremia after starting it.