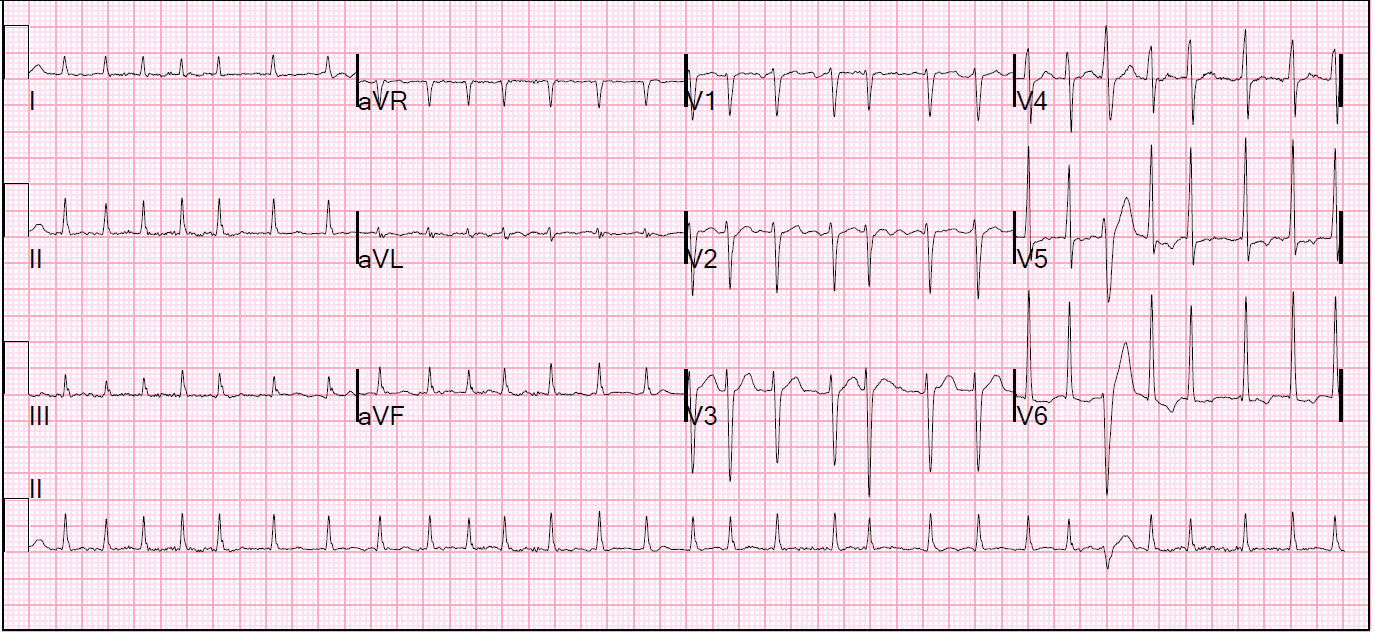
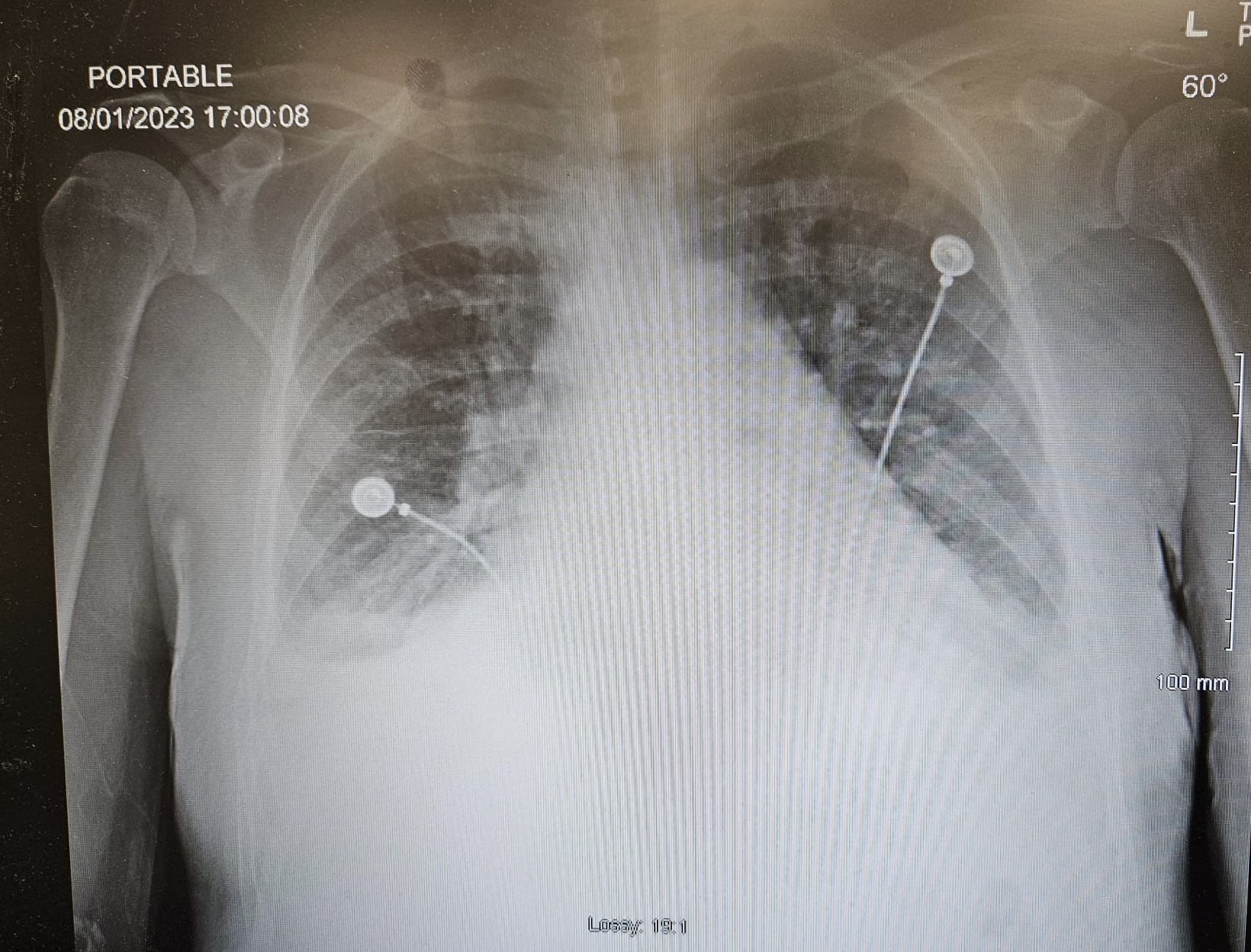
Case Presentation: A 39-year-old male with no significant past medical history presented to the ED with dyspnea on exertion, palpitations, orthopnea, lightheadedness, anxiety, 100-pound weight loss over a 2-year period, and swelling in his left lower extremity. Upon admission, the patient was tachycardic and tachypneic. EKG was significant for new onset atrial fibrillation with RVR, rate 173 bpm, with T wave inversion in lateral leads. Cardizem bolus and drip were initiated for atrial fibrillation. However, once chest x-ray showed pulmonary vascular congestion and bilateral pleural effusions concerning for CHF, cardizem drip was stopped. CTA of the chest confirmed earlier findings. Within the initial hours of admission, the patient’s respiratory status worsened and he became agitated, diaphoretic, and hypoxic with O2 saturations dropping to 88%. TSH was severely low at < 0.050 and free T4 was elevated at >8. Thyroglobulin antibody and thyroid peroxidase antibody were ordered. Overnight, the patient was treated with IV steroids, propranolol, breathing treatments, placed on BiPAP, and subsequently transferred to the ICU with improvement in respiratory status. The following day, a transthoracic echocardiogram was done, showing an ejection fraction of 25 to 30%. Patient was subsequently initiated on GDMT while continuing the course of treatment for thyrotoxicosis. By discharge, TSH levels had significantly improved and immunology results had finally resulted, revealing thyroglobulin antibody at 103 (reference: 0-4) and thyroid peroxidase antibody at 2182 (reference: 0-9). Patient was discharged on methimazole for Graves’ disease. LifeVest was also provided with instructions to follow-up at the free clinic by cardiology. Per follow-up, it was determined that the patient had experienced two rounds of ventricular tachycardia. Months later, repeat TTE showed improvement in EF and LifeVest was discontinued.
Discussion: An unchecked overactive thyroid, if not tested appropriately, can lead to life-threatening arrhythmias that may cause structural changes in the cardiovascular system. This particular case demonstrated the effects of thyrotoxicosis in the setting of Grave’s disease, which lead the patient to experience both atrial fibrillation and ventricular tachycardia. Over time, as the patient’s hyperthyroidism went untreated, he developed dilated cardiomyopathy with echocardiogram revealing an EF of 25-30%. In regards to the incidence of heart failure in patients with hyperthyroidism, Siu et al. shows that in patients with hyperthyroidism, approximately 6% initially present with signs of congestive heart failure (3). In our patient, once placed on the appropriate anti-thyroid medication and beta-blockers, his symptoms improved and EF improved three months down the line. Eliades et al demonstrated similar effects in regards to improvement in cardiac function when thyroid levels were appropriately treated (2).
Conclusions: Overall, this case demonstrates several learning points. First, hyperthyroidism is becoming more common and there is a need to have thyroid levels monitored appropriately in the adult population. If hyperthyroidism goes unchecked, it can lead to life-threatening arrhythmias that may essentially have unfortunate cardiac outcomes. Dilated cardiomyopathy can develop secondary to thyrotoxicosis; however, once placed on the anti-thyroid, medication, and beta blockers, thyroid hormone levels may normalize, which, in turn, may reverse the cardiomyopathy.