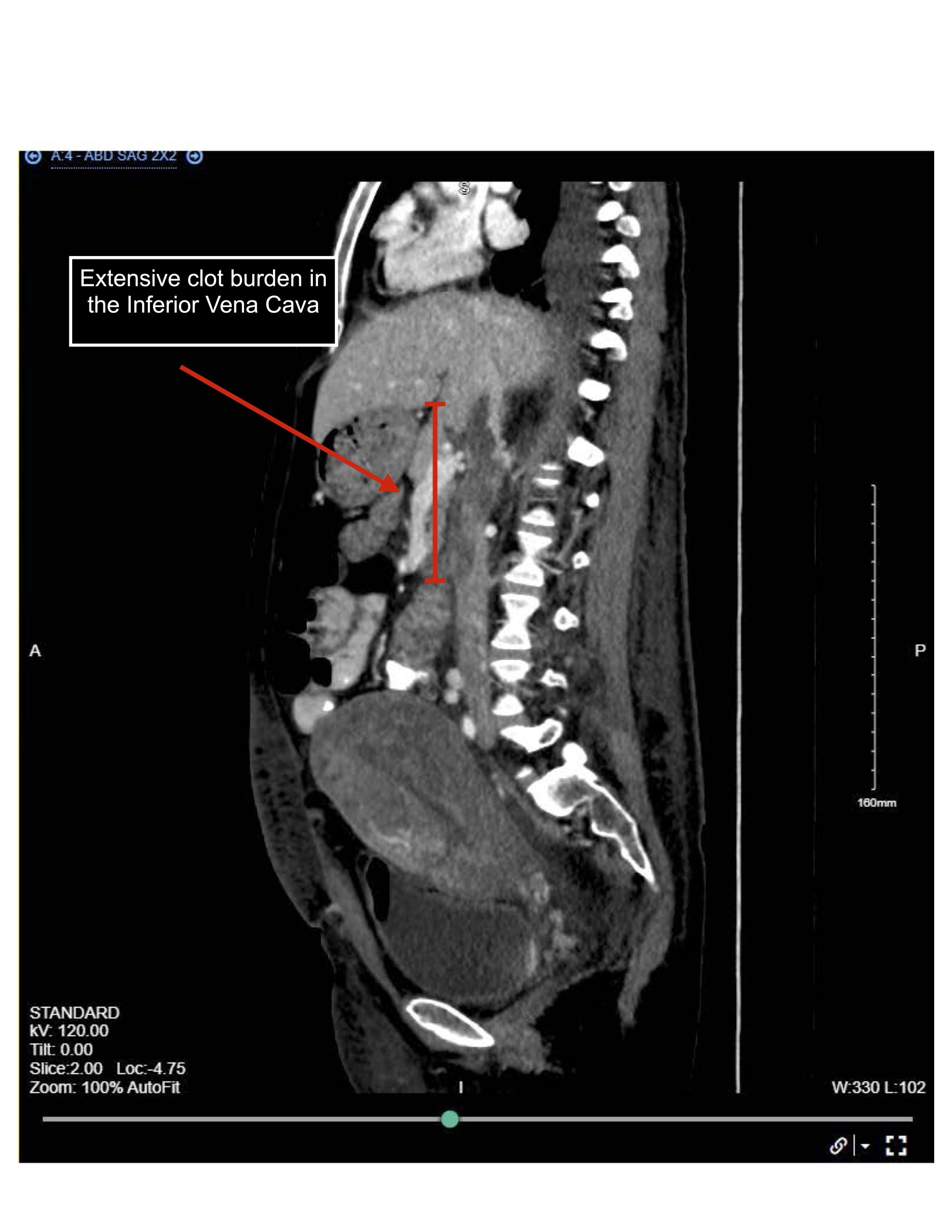
Case Presentation: A 31-year-old woman, G2P1A0, 32 weeks pregnant, with a history of systemic lupus erythematosus (SLE), presented with a gradual onset of worsening abdominal wall, genitalia, and bilateral lower extremity swelling. Upon admission, the workup revealed nephrotic-range proteinuria, normal renal function, and elevated anti-dsDNA. A lower extremity ultrasound showed no evidence of deep vein thrombosis. A presumptive diagnosis of membranous lupus nephritis was made, and she was initiated on high-dose steroids and azathioprine. However, a week after admission, edema and proteinuria continued to worsen despite immunosuppressives and diuresis, leading to the decision to deliver the baby. On the second day postpartum, she developed a fever and became tachycardic and hypotensive. A CT abdomen/pelvis revealed a thrombus in the inferior vena cava (IVC) extending to renal and gonadal veins with a massive pulmonary embolism (PE). Therapeutic enoxaparin was started. Infectious and antiphospholipid syndrome workup yielded negative results. The fever was attributed to venous thromboembolism (VTE), and hypotension was thought to be secondary to decreased venous return. later, she was discharged on azathioprine and apixaban. During outpatient follow-up, there was a significant improvement in peripheral edema and a reduction in proteinuria. A renal biopsy was deferred due to the recent diagnosis of deep vein thrombosis (DVT), ongoing anticoagulant use, and the improvement in proteinuria on empiric therapy.
Discussion: IVC thrombosis is rare, accounting for 1.3% of diagnosed VTE cases in hospitalized patients in the United States [1]. Due to its rarity and the nonspecific nature of symptoms, underdiagnosis is common, especially in those with coexisting nephrotic syndrome due to overlaps in symptoms. Clinical presentations can range from asymptomatic cases to severe cardiovascular collapse, depending on the extent of thrombus extension [2]. Symptoms arise from blood pooling within the IVC and reduced venous return to the heart [3]. Unfortunately, there is no single specific symptom or test for differentiation, however, there are some clues that should raise concern for presence of IVC thrombus in patients with nephrotic syndrome such as unexplained pelvic or back pain, caput medusa, edema resistance to diuretics, bilateral LE DVT, recurrent DVT or PE, an unretrieved IVC filter, manifestation of cardiovascular decompensation, or presence of other predisposing factors for VTE such as pregnancy or SLE. IVC thrombus can be readily detected by CT with IV contrast or MRI, with CT with 80% sensitivity rate [4]. Treatment approaches vary based on the cause and severity. Initial treatment typically involves systemic anticoagulation, with catheter-directed fibrinolytic or mechanical thrombectomy considered for select case.
Conclusions: IVC thrombosis is rare, challenging to diagnose, and particularly complex in patients with coexisting nephrotic syndrome. This case highlights the importance of considering IVC thrombosis in high-risk patients and underscores the need for a low threshold for imaging in those with predisposing factors for venous thromboembolism.