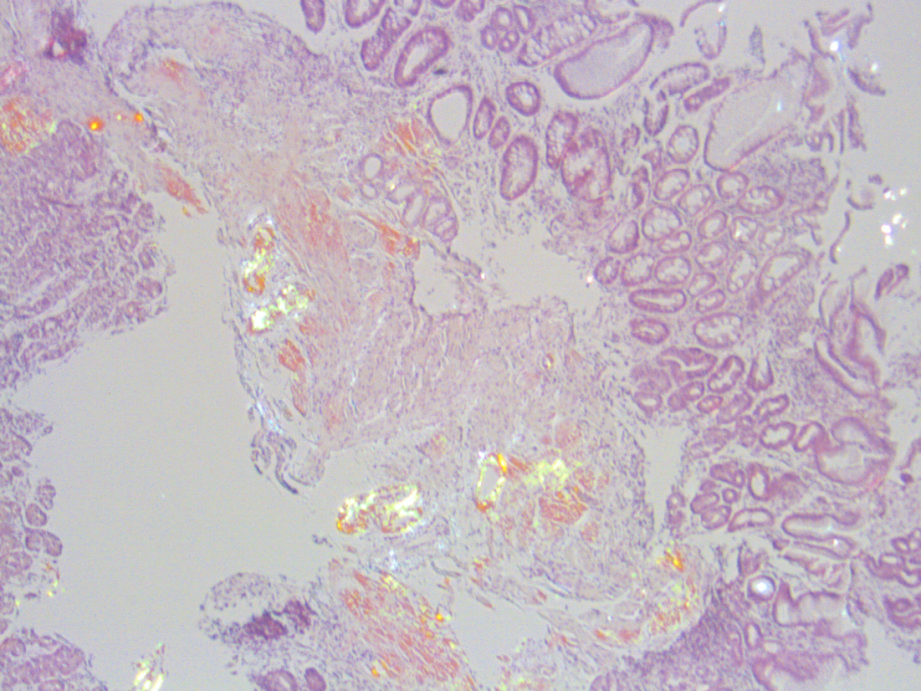
Case Presentation: A 82 year old Caucasian male with history of long standing well controlled diabetes mellitus type 2 since 2010, gastroparesis, and GERD presented to the ED with 2 episodes of “dark, tarry” stools for 1 day onset with resolution. On review of systems, the patient endorsed 32 pound weight loss over 6 months, decreased appetite and fatigue. He denied fever, chills, night sweats, nausea, vomiting, hemoptysis, chest pain, dyspnea. The patient was hospitalized 6 months prior for postprandial RUQ abdominal pain with subsequent EGD that was unremarkable. A gastric emptying studying also demonstrated decreased emptying and was said to be consistent with diabetic gastroparesis. His glycosylated hemoglobin A1c (HgbA1c) was 5.5. Initial physical exam was remarkable for stage 2 hypertension. He had no orthostatic hypotension or abdominal tenderness. His initial labs were remarkable for hemoglobin of 11.0 mg/dL, WBC of 6.7 mg/DL. His total serum protein was 6.3 g/dL, albumin was 3.2 g/dL with a protein gap of 3.1, and ALK of 66 U/L with all other labs unremarkable . An EGD was performed which showed 2 linear superficial lesions with adhere blood in the proximal gastric body with no ulceration or active bleeding (image 1). Stomach biopsy demonstrated metaplastic atrophic gastritis with negative Helicobacter pylori immunohistochemistry staining. Further analysis with Congo-red cytochemical stain showed apple-green birefringence in scattered amorphous hyalinized deposits persistent in the lamina propria, muscularis mucosae, and vascular tissue indicating the presence of amyloidosis. Liquid chromatography-tandem mass spectrometry detected amyloid light-chain (AL), lambda-type (image 2). The patient was placed on lenalidomide (revlimid) and dexamethasone. Unfortunately, our patient eventually developed persistent heart failure symptoms of edema and dyspnea as well as severe labile orthostatic hypotension despite being placed on fludrocortisone and midodrine. He also developed intolerable nausea and fatigue from revlimid within 6 months of diagnosis leading to hospice.
Discussion: Our patient experienced melena as his initial presenting symptom that prompted diagnosis of AL amyloidosis, which is only found in 1% of patients. Our patient also had a significant 32 pound unintentional weight loss, early satiety, and right upper quadrant abdominal pain 6 months prior to his hospitalization. At that time, his symptoms were attributed to gastroparesis secondary to type 2 diabetes mellitus. However, his hgbA1c was 5.5 at that time and has been well controlled since 2010. Our patient’s symptoms of gastroparesis in light of well controlled type 2 diabetes mellitus should also prompt additional etiologies. In fact, while up to 30% of patients with long standing (≥ 10 years) type 2 diabetes mellitus can develop gastroparesis, this is more prevalent in those with higher glycosylated hemoglobin (HbA1c), body mass index, and poorly controlled glycemic index. Since our patient’s HbA1c was well controlled, his gastroparesis may have also been secondary to an additional unknown underlying etiology, later thought to be due to a neuromuscular process from amyloidosis discovered on gastric biopsy.
Conclusions: This case demonstrates the importance of maintaining clinical suspicion of other etiologies of gastroparesis in the setting of well controlled type 2 diabetes mellitus and gastrointestinal involvement. Without early detection and treatment, AL amyloidosis can result in death within 2 years in 80% of patients.