Background: Mentorship is a key element of success in physicians’ career advancement, satisfaction, and avoidance of burnout. Conversely, lack of mentorship is a contributor to dissatisfaction, especially among those who leave the field. Mentors act as guides for professional development; there are several benefits of successful mentoring relationships to both parties. While classically enjoyed by faculty on the physician-scientist (traditionally, tenure-granting) track, the principles and benefits of mentorship are broadly applicable, including to those junior faculty on the clinical track who primarily teach and care for patients.
Methods: Our institution established the Clinician Mentoring Program in 2019. For all clinical track faculty of academic rank below Clinical Associate Professor, a mentoring committee is formed. Committees are comprised of one chair (usually the section chief or chief of medicine) and three to six members, chosen by the mentee and chair. Other mentors include leaders within the healthcare system or from the quality improvement, education, policy, or other domains in which the mentee is interested.Committee meetings generally occur twice a year for one hour. A project manager coordinates and assists with meeting materials, including distribution of the mentee’s CV before the meeting. The mentee is expected to be familiar with general mentee guidance (“The Four Golden Rules of Effective Menteeship”1) and promotion information, both of which are sent prior to the first meeting along with meeting structure expectations. During meetings, the mentee and chair guide conversation, which spans the mentee’s short-, mid-, and long-term goals, assessment of personal and professional satisfaction, updates in areas in which the mentee is spending time, and ideas on how the committee can better help the mentee. Following each meeting, feedback from all participants is collected using a standardized assessment tool that we developed called the Mentorship Meeting Assessment Tool (MMAT). This anonymous, web-based, Likert scale survey elicits information on meeting logistics, perceptions of feedback receipt, clarity of next steps, assessment of progress, and impacts of the program on satisfaction and burnout.
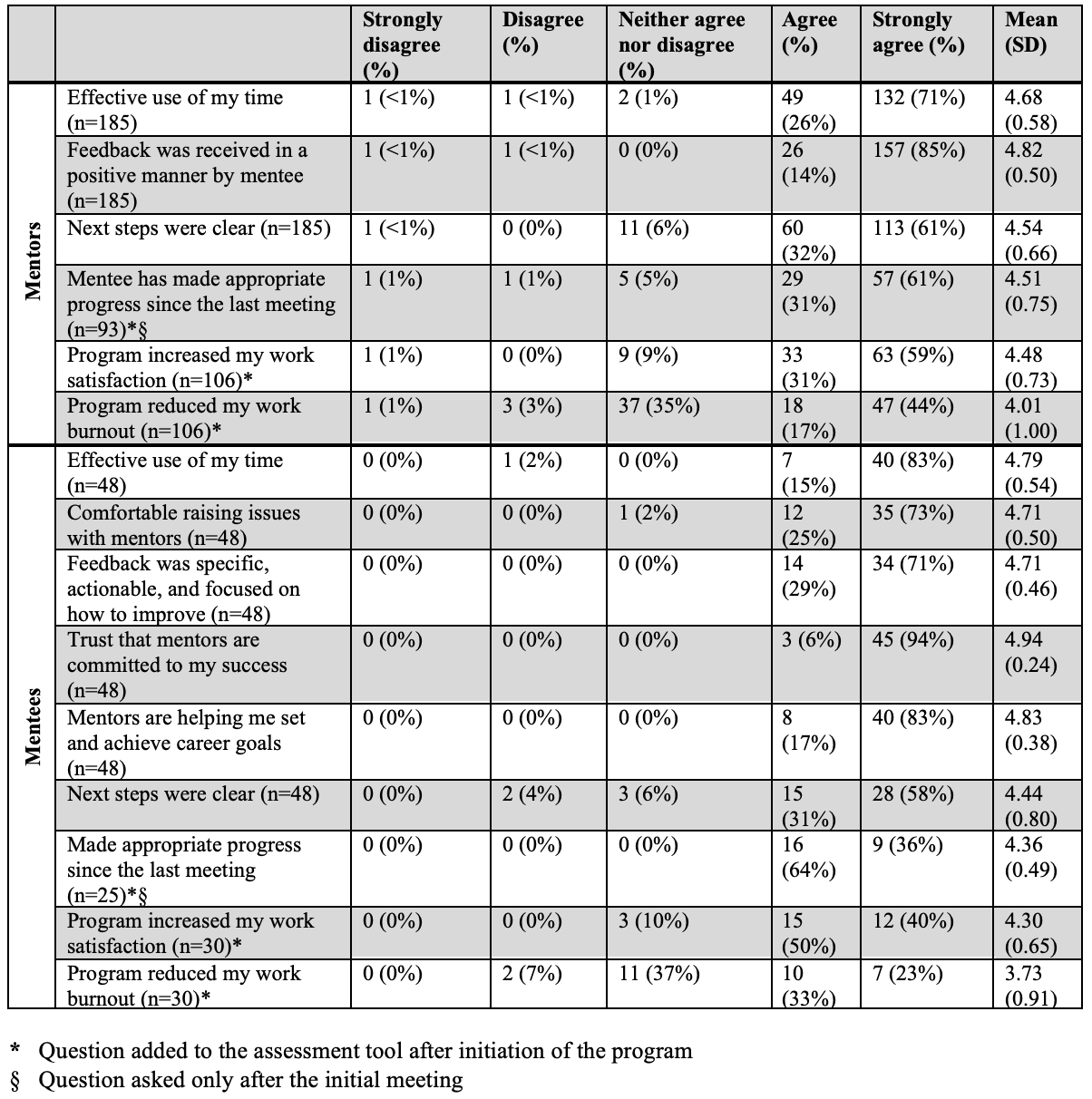
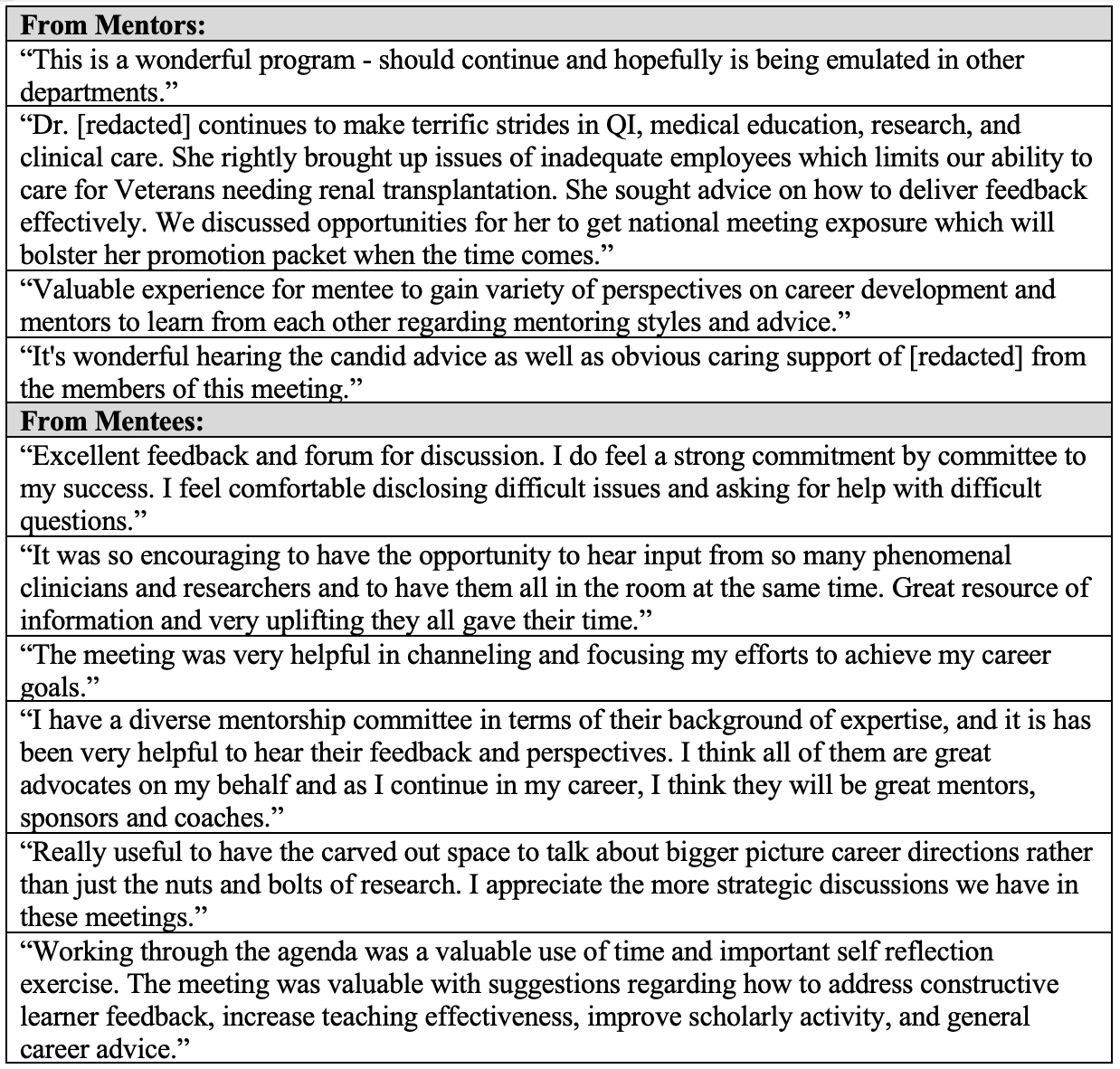
Results: To date, the program has enrolled 25 mentees from 10 unique clinical sections (32% within Hospital Medicine) in which 48 distinct meetings have occurred. Overall response rate to the MMAT was 100%. Three of 25 (12%) mentees were promoted to the rank of Clinical Associate Professor, and of those remaining, 21 of 22 (95%) continue in the program. Perceptions of the program and its impacts on participants collected from both mentors and mentees are in Table 1. Total numbers of responses differ because some questions were added to the assessment tool after initiation of the program and some were asked only after the initial meeting. Mean scores from 1 (strongly disagree) to 5 (strongly agree) with standard deviations are reported. Selected participant comments are in Table 2.
Conclusions: A structured mentoring program targeted to clinician educators has been preliminarily successful in helping junior faculty get promoted. Further, the program is viewed positively by both mentees and their committee members. In fact, for many participants, the program led to enhanced work satisfaction and reduced burnout. Hospital Medicine programs may consider establishing formal mentoring programs for clinically oriented faculty to foster their professional development.