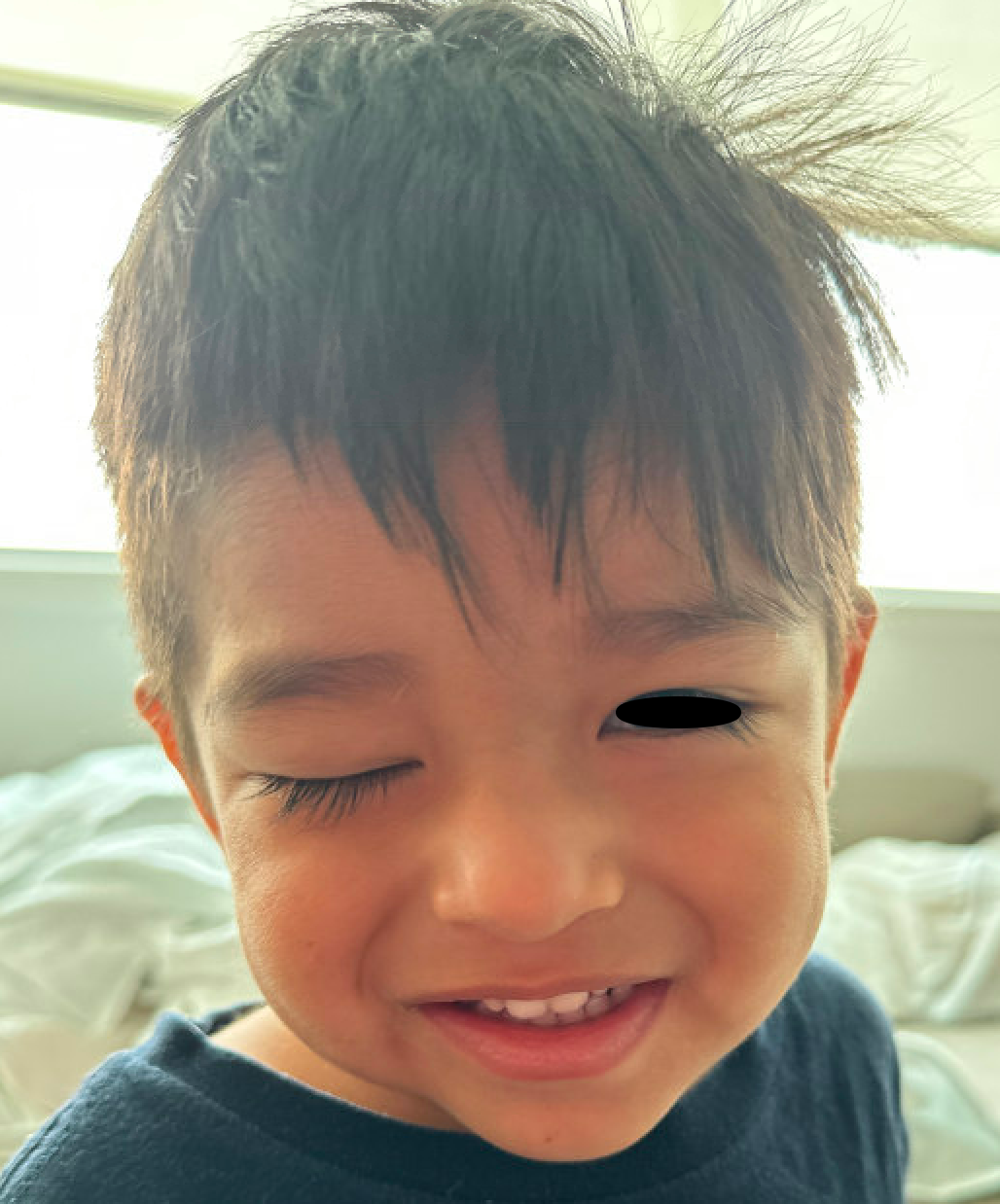
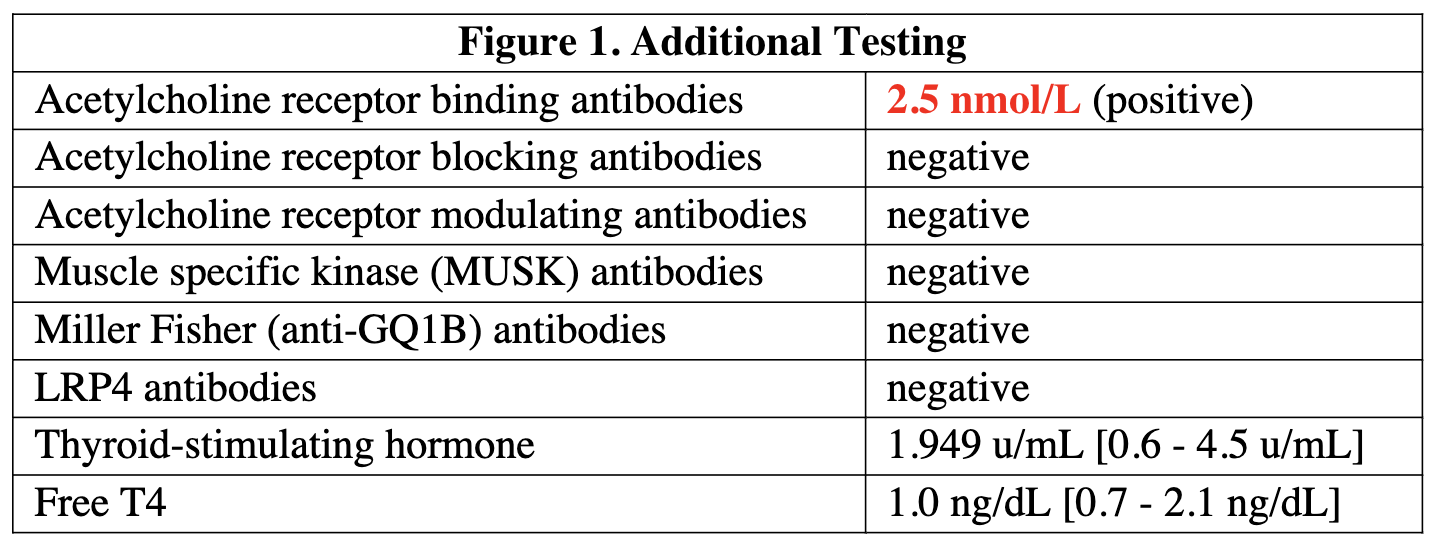
Case Presentation: A previously healthy two-year-old male presented with six days of painless right ptosis, fever, cough, and nasal congestion. He had no ocular or head trauma. He had tried antihistamines without benefit. Non-contrast CT head showed only paranasal sinus disease. See Image 1.He was evaluated by Neurology and Ophthalmology and found to have complete right ptosis and inability to abduct the right eye. MR of the head showed normal cranial nerves and MR angiography was normal. During admission, he demonstrated mild improvement of ptosis upon waking that worsened throughout the day. Acetylcholine receptor binding antibodies were positive. See Table 1 for additional tests.The patient was followed in Ophthalmology and Neuromuscular clinics. His right ptosis continued, and he subsequently developed near-complete left ptosis. Sedated electromyography (EMG) of the trapezius and abductor pollicis longus was consistent with post-synaptic neuromuscular junction transmission dysfunction; however, the parents reported no upper or lower extremity weakness or limitation in the patient’s activities other than that caused by his ptosis.Pyridostigmine therapy was initiated and titrated up to 1 mg/kg QID and prednisone 1mg/kg daily was added. He continued to have minimal right ptosis on this regimen to which he was able to adapt using a chin-up posture. He has had no voice change, dysphagia, shortness of breath, or difficulty ambulating.
Discussion: Elevation of the eyelid requires joint action of the levator palpebrae superioris muscle (via innervation from CN III), the superior tarsal muscle (via sympathetic nerves), and indirectly the frontalis muscle (via CN VII). Abduction of the eye relies on the lateral rectus muscle (via CN VI). This case highlights the importance of a thorough ophthalmologic exam in patients with ptosis, as closure of the eye can mask cranial nerve deficits. A central cause of ptosis (including mass or venous sinus thrombosis) was initially considered for this patient but ruled out with imaging. An isolated CN III lesion would typically also cause a deficit in supraduction of the ipsilateral eye, which our patient did not have. His ptosis and isolated right abduction palsy did not co-localize, bringing neuromuscular junction disorders including juvenile myasthenia gravis (JMG), Miller-Fisher, and Lambert-Eaton to the top of the differential. It is unclear whether the patient’s development of JMG was related to his concurrent viral upper respiratory tract infection, as his symptoms had not abated in the intervening five months.Many patients with JMG will exhibit ocular symptoms at presentation and later develop weakness of the extremities. A small proportion will continue to have only ocular symptoms. While our patient’s parents did not note any limitation of his activities due to extremity weakness, EMG testing in fact showed that muscles throughout his body were affected. Timely diagnosis allowed us to provide our patient’s family with strict return precautions for respiratory depression or extremity weakness. Additionally, we hope that aggressive medical management and close Ophthalmology follow up will prevent this patient from developing amblyopia as a result of his ptosis. Future treatment may include immunosuppressive agents or thymectomy.
Conclusions: Myasthenia gravis, both ocular and generalized, is rare in young in children but should be considered in the differential diagnosis for any patient with new onset ptosis. An ophthalmologic exam is warranted for such patients.