Background: As COVID-19 spread across the globe, hospitals restricted visitors in an attempt to protect patients and healthcare providers. The absence of in-person visitors and loved ones, who play a central role in clinical decision-making by clarifying medical histories, elucidating patients’ baseline status, and bridging linguistic and cultural divides, left patients vulnerable to social isolation, delirium, and fragmented clinical care. On the frontlines of the pandemic, hospitalists and trainees grappled with how to support their patients experiencing isolation and keep them connected with outside support systems.
Purpose: To reduce patient isolation and keep loved ones involved in clinical care delivery during COVID-19 visitor restrictions, trainees rapidly developed and implemented a telehealth initiative, Connecting During COVID across three different affiliated hospitals. The SHIFT-Evidence quality improvement framework guided the design and implementation of this initiative.
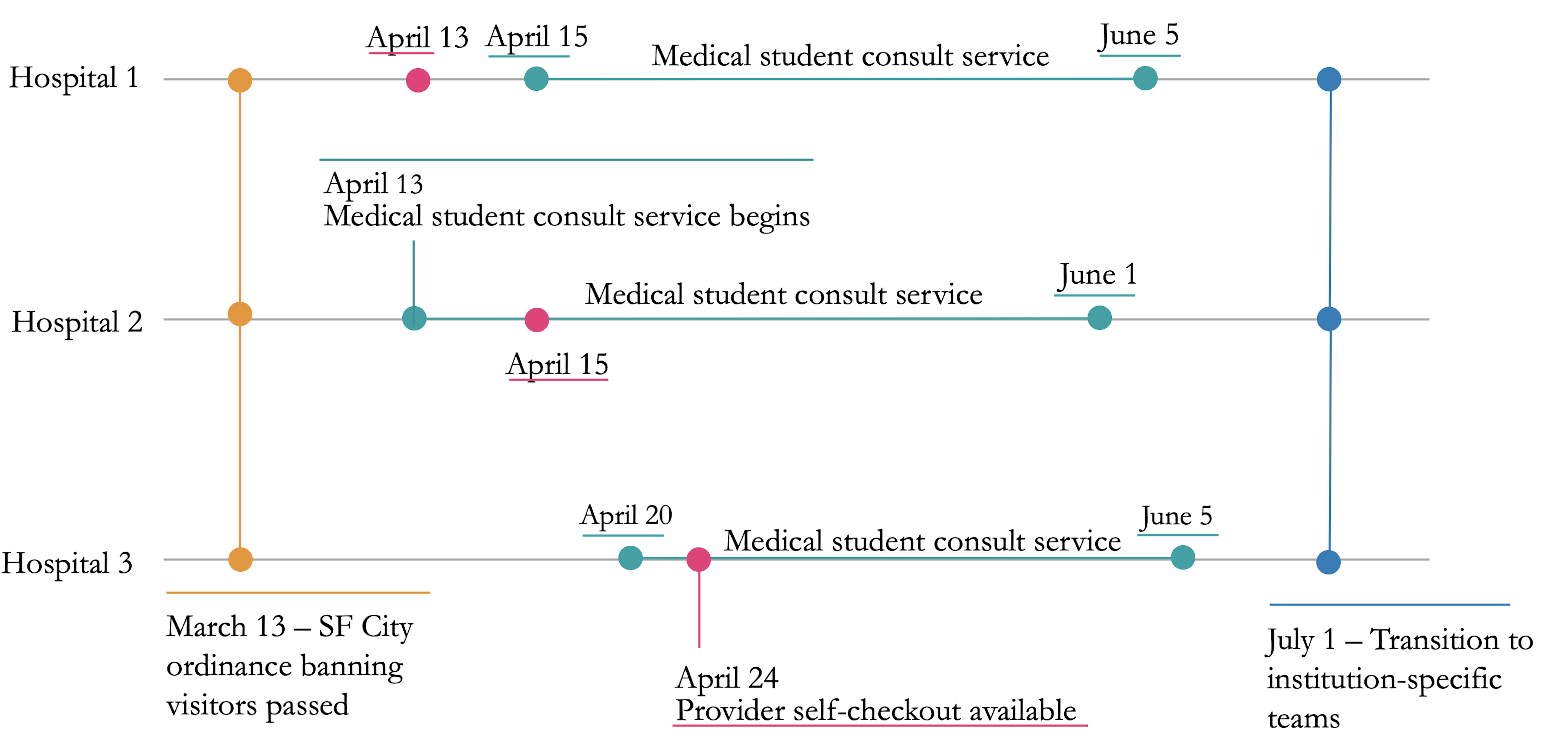
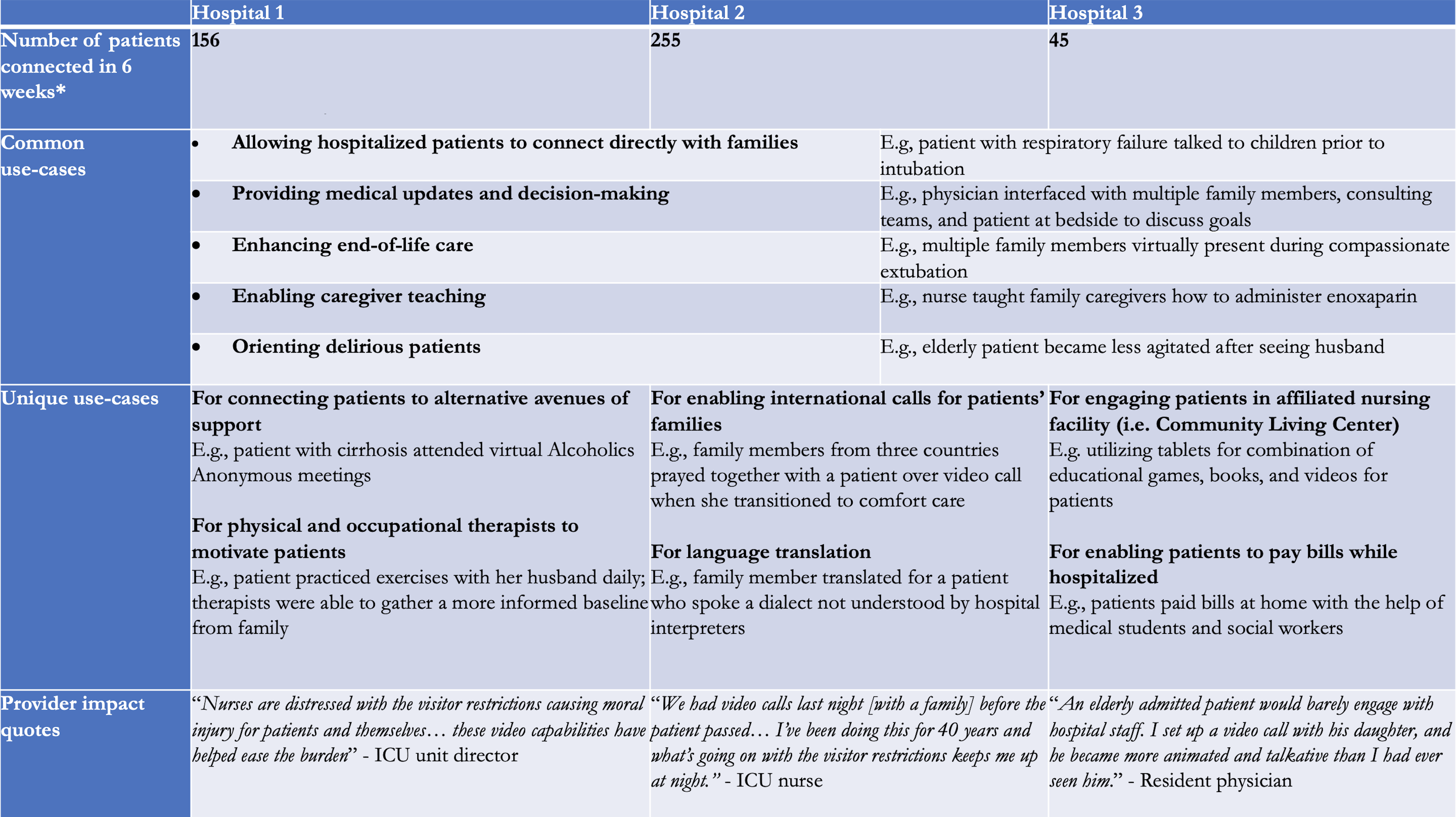
Description: Within three weeks of a city-wide ban on hospital visitors in March 2020, a group of trainees, including internal medicine resident physicians and medical students, rapidly developed an inpatient telehealth program designed to keep hospitalized patients and loved ones connected across three hospital systems where medicine residents rotate. We solicited private tablet donations and loaded hardware with requisite security software at each site. We chose Zoom as the primary video conference platform based on privacy, security, and familiarity among patients and loved ones. To maximize use of a limited number of tablets and minimize staff training, we created medical student-led consult teams to coordinate video visits for patients. Any clinician could page the consult team during business hours. The consult team coordinated with the patient and their loved ones to obtain consent, download and troubleshoot Zoom, schedule an appointment time, and physically set up the tablets. In response to requests for after-hour consults, we developed a provider-driven self-checkout workflow for trainees, hospitalists, and nurses to checkout tablets on-demand (Figure 1). Over 450 video visits were completed by early June, which accounted for 190 unique patients (Table 1). Given the program’s success and the ongoing need, one of the health systems provided staffing for 2 FTE of two inpatient video visit navigators to be able to coordinate video visits daily from 8AM – 8PM daily.
Conclusions: This innovation report highlights the role of trainees in improving clinical care delivery and can serve as a model for hospitalists looking to partner with trainees to create a sustainable inpatient telehealth program to connect hospitalized patients and their loved ones.