Background: At our 583-bed tertiary care nonprofit teaching hospital serving the greater metropolitan New York area, ESRD (End-Stage Renal Disease) patients on hemodialysis presenting with complaints like chest pain, shortness of breath, hypertensive urgency, pulmonary edema, would sometimes wait for more than 6 hours to get dialysis started. While they were “waiting” to get admitted some of these patients would often decompensate, needing higher level of care. As part of our hospital practice, dialysis patients need to be admitted before dialysis orders can be entered. The “waiting” time for admission was impacted by the ED (Emergency Department) finding an accepting Medical attending, waiting for the MICU (Medical Intensive Care Unit) team to evaluate the unstable patient, communicating with the bed board team regarding the type of bed needed, and finally the time taken to secure a bed.
Purpose: To ensure timely dialysis for ESRD patients needing it on admission
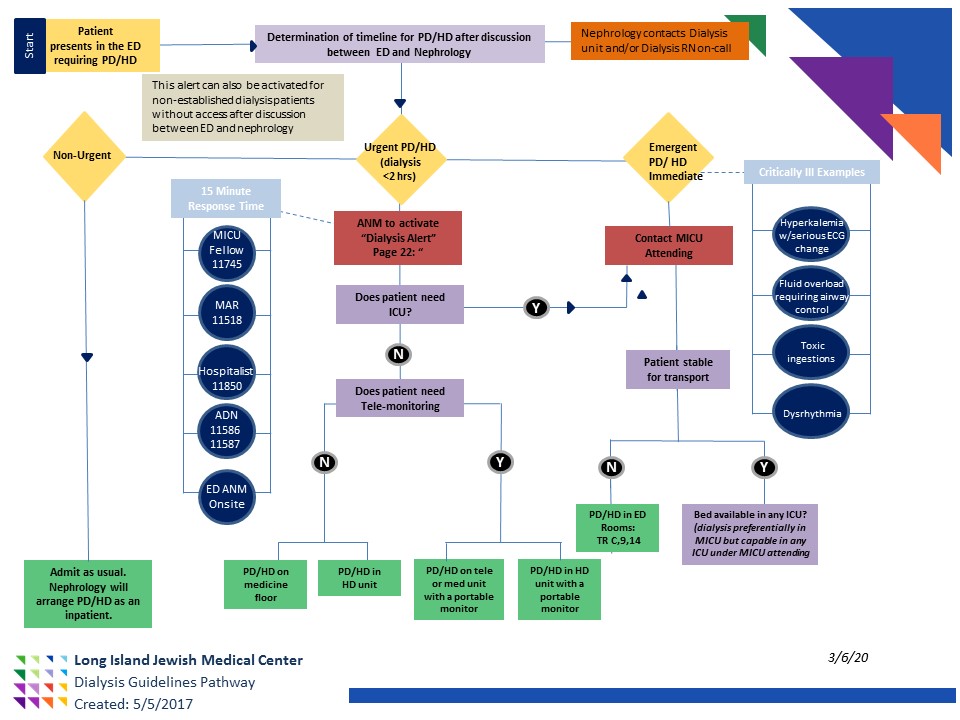
Description: One of our Nocturnists (night hospitalist) escalated this issue after 2 patients decompensated and needed to go to the MICU. A working group including Hospitalists, Intensivists, ED physicians, Nephrologist, and Nursing from ED, Medicine Nursing, and Dialysis Unit was created in 2017 to help streamline the admissions process for ESRD patients who were presenting with complaints that can be alleviated with dialysis being initiated shortly after arrival to the ED. After several meetings, the team proposed a “Dialysis alert” to be activated once the Nephrologist and the ED physician discussed the timeline for dialysis. The alert would only be activated if that discussion clarified that the patient would benefit from dialysis within 2 hours. The Hospital Communications department sends a page or a call to 5 team members who huddle at the bedside of the patient to have a collaborative discussion regarding the disposition of the patient- a floor bed, a telemetry bed, or a MICU bed. The 5 members are: HIC (Hospitalist-in-charge), ADN (Assistant Director of Nursing), MAR (Medical Admitting Resident), MICU fellow, and ER Nursing/team. They evaluate the patient at the bedside, in unison, and once a disposition is decided, the ADN expedites the bed, while the Nephrologist contacts the Dialysis unit staff to set up the dialysis apparatus. The HIC serves as the accepting admitting physician, especially during off hours as finding an accepting Voluntary attending could take longer, thereby decreasing the time to admission. The care of the patient is appropriately transferred once the it is determined if the Voluntary attending will accept the patient. This proposal was presented to Hospital Leadership and approved.
Conclusions: Prior to the Dialysis Alert, waiting for an accepting admitting attending or waiting for the MICU consult evaluation to determine where the patient would be admitted led to delays of up to 6-8 hours for dialysis, that then contributed to worsening of the symptoms and possible re-evaluation and admission to the ICU.This alert went live in 2017 and is activated approximately 2-4 times a month. The goal time of dialysis within 2 hours of admission is being met for 20/39 (51%) of patients. Delays of more than 2 hours were due to dialysis alert being activated without the Nephrologist being involved or the patient not having dialysis access. The working group started meeting regularly in 2020 to continue to work on ways to improve the throughput and safety of our ESRD patients, both on HD and PD (Peritoneal Dialysis).