Case Presentation: An otherwise healthy 23-month-old girl presented to her pediatrician with several days of vomiting, abdominal pain, and decreased oral intake. She was found to have a Sodium of 128 mmol/L with mild transaminitis. She was admitted, treated IV fluid, had improvement in her sodium and oral intake and discharged after two days.
She returned the following day due to facial swelling but was otherwise clinically improving. Her vitals were stable and physical exam was significant for periorbital edema, 2+ pitting edema of both lower extremities, mild oral pharyngeal erythema, diminished lung sounds at the bases, and a slightly distended but soft abdomen.
Labs were significant for a Sodium of 133 mmol/L, Albumin of 1.7 g/dL, Prealbumin of 9 mg/dL, total protein 3.1 g/dL, Creatinine of 0.2 mg/dL, and a Urinalysis without proteinuria. LFTs were normal except for an ALT of 43 IU/L.
Abdominal US showed ascites, small bilateral pleural effusions, normal kidneys and mild splenomegaly. An ECHO showed normal biventricular normal function. A Fecal Calprotectin, Celiac screen, ESR/CRP, EBV titers, Giardia, and H.Pylori stool antigen were negative. Total IgG was low but IgM and IgA were normal. A food allergy panel was negative except for elevated IgG to eggs. Fecal Alpha-1 antitrypsin and CMV IgM and IgG levels were positive.
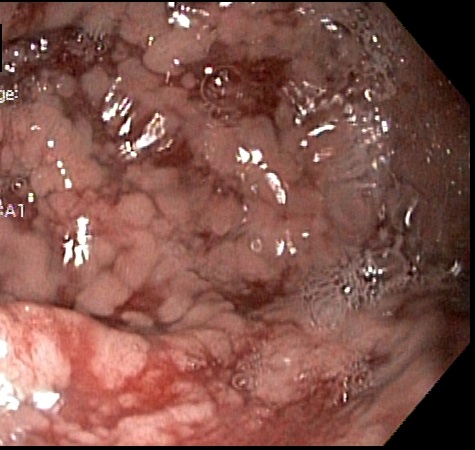
An EGD showed a normal esophagus, but congested, erythematous and friable mucosa in the gastric body. A flexible sigmoidoscopy was overall normal. Gastric biopsies were significant for marked foveolar hyperplasia, lamina propria edema and chronic inflammation consistent with Ménétrier disease.
Discussion: Ménétrier Disease, also called Giant Hypertrophic Gastropathy, is a rare cause of protein-losing enteropathy, edema, and hypoalbuminemia in the pediatric population. These patients commonly present with vomiting, abdominal pain, diarrhea, and edema of several days to weeks duration. In contrast to adult onset, the pediatric form tends to be self-limiting, lasting 4-6 weeks on average. This is most commonly associated with CMV infection, although less commonly observed with H.Pylori, Salmonella, and Giardia infections.
The pathophysiology of Ménétrier disease, and the resulting gastric inflammation, is not completely understood. This inflammation causes a widening of tight junctions between gastric cells, allowing the flow of proteins into the gastrointestinal tract. Ménétrier disease is commonly diagnosed by enlarged gastric rugae visualized either on endoscopy or other imaging. Treatment is typically supportive, with albumin infusions and Lasix, or an H-2 Blocker. Occasionally, a course of Gancyclovir is indicated.
Conclusions: This case illustrates the importance of considering Ménétrier disease as one of the causes of a protein-losing enteropathy in the pediatric population. While other causes, such as celiac disease or IBD may be more common, hypoalbuminemia with a viral prodrome and gastrointestinal symptoms can be related to Ménétrier disease. A majority of the literature on Ménétrier consists of previous case reports and literature reviews.