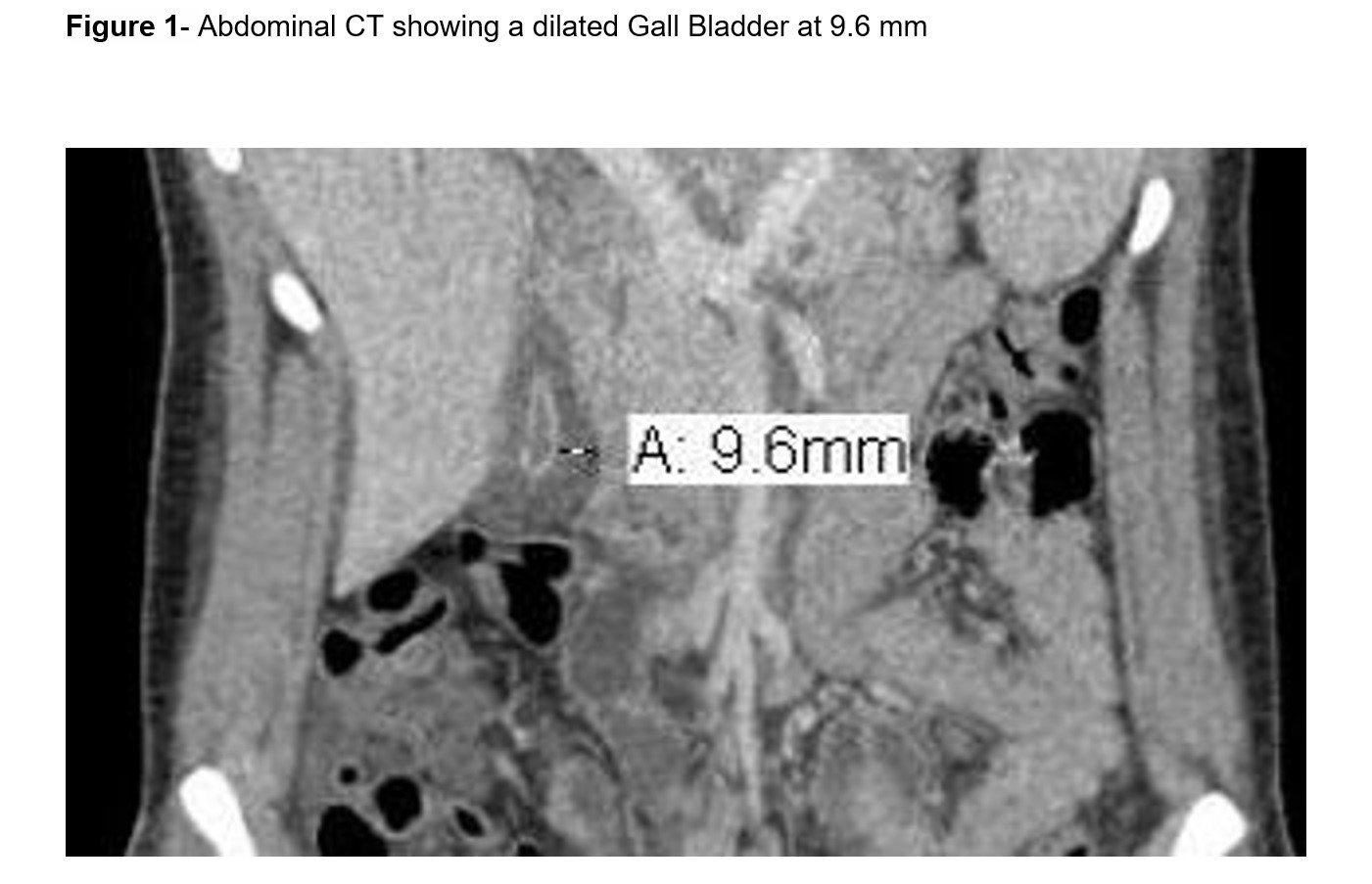
Case Presentation: An 18 years old female with no significant medical history was initially admitted to an outside hospital for urinary tract infection with sepsis. She subsequently developed abdominal pain and elevated liver enzymes prompting transfer to our institution. Physical examination consistent with right upper quadrant pain but remainder was unremarkable. Laboratory testing revealed a total bilirubin 6 mg/dl, Alk phosp 262 U/L, AST 429 U/L, ALT 305 U/L, and WBC 11.5 per microliter. CT showed a 9.6 mm gallbladder wall thickening, and pericholecystic fluid (Figure 1). HIDA scan showed a patent biliary system and endoscopic ultrasound showed no evidence of stone or sludge. HIV, RPR, Chlamydia-Gonorrhea, Hepatitis panel, CMV, ANA, AMA, and ASMA were negative. Immunoglobulins, iron profile, and ceruloplasmin levels were normal. Ebstein-Barr Virus (EBV) PCR was positive at 1384 copies/ml so acalculous cholecystitis (ACC) secondary to EBV infection was felt to be the likely diagnosis. Surgery was consulted and advised for conservative management. She clinically improved and was discharged home.
Discussion: ACC accounts for approximately 10% of all cases of acute cholecystitis and is typically seen in critically ill patients in the setting of an infection. The diagnosis of acute ACC is made based on clinical symptoms, laboratory tests, and imaging. A review by Barie et al. noted a strong male predominance among patients with ACC (80%). However, the majority of 26 reported cases in medical literature for ACC secondary to EBV infection were females. In these patients, hyperbilirubinemia and moderate transaminase level elevation were the most common laboratory findings. Serologic testing and EBV PCR are used to confirm the presence of infection. In all the reported cases, including our patient, ACC subsided during the regression of the EBV infection without the need for surgical intervention.
The etiology and pathogenesis of ACC remains uncertain. Abdominal US is considered as an effective tool to confirm diagnosis. In our patient the diagnosis was made based on CT and confirmed with HIDA and EUS. The main radiographic diagnostic criteria supporting ACC is the absence of gallstones, in addition to at least of two of the following findings: wall thickness over 3 mm, gallbladder distention, pericholecystic fluid, and mucosal membrane sludge. Our patient had a 9.6 mm wall thickening, with the presence of pericholecystic fluid and absence of gallstones. Our case report confirms the favorable prognosis and self-limiting nature of a primary EBV infection, even in the presence of ACC.
Conclusions: Acute EBV infection is a rare but established etiology for ACC and should be considered in the differential diagnosis for female patients presenting with acute ACC.