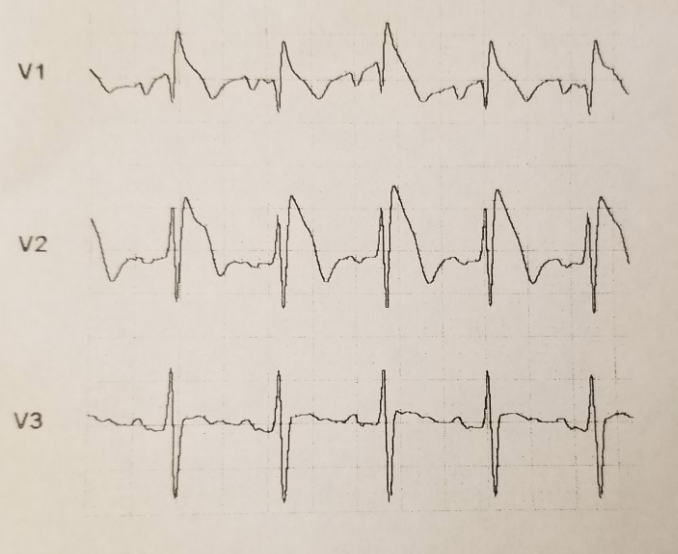
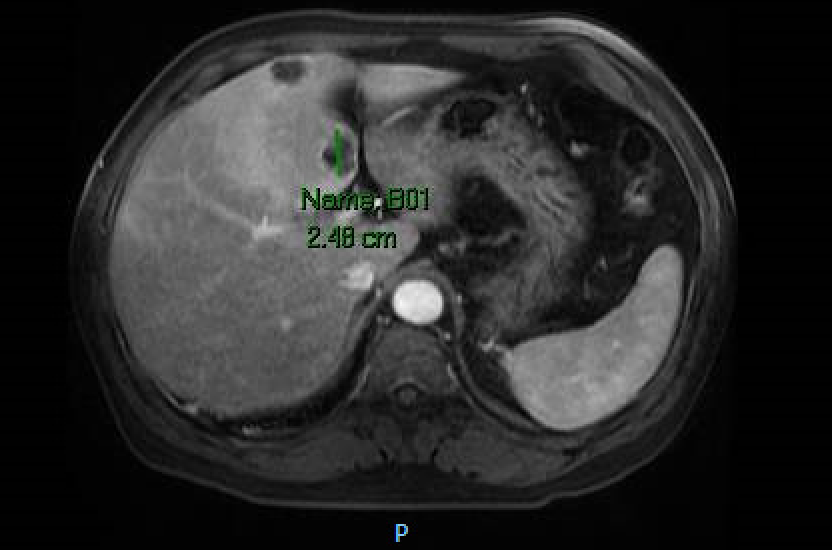
Case Presentation: A 55 year-old Korean male with a past medical history of hypertension and hyperlipidemia presented to the Emergency Department after feeling short of breath with chest pain, palpitations, mottled skin and blue lips. He endorsed five days of fever, headache, shortness of breath, abdominal pain and nausea. He denied recent travel and sick contacts. He was febrile to 101.6ºF and on examination was diaphoretic, tachycardic to 139 bpm and tachypneic to 36 breaths/minute. Blood work showed transaminitis (AST 82 and ALT 139 u/L) along with elevations in alkaline phosphatase (139 u/L), lactate (2.6 mmol/L) and GGT (280 u/L). Initial EKG taken by EMS revealed a Brugada pattern (ST elevations in V1-V3 with right bundle branch block [RBBB]). He was admitted and treated for severe sepsis. Repeat EKG showed persistent RBBB with resolution of ST changes. Chest X-ray, respiratory viral panel and urinalysis were unremarkable. Cardiac enzymes were negative and echocardiogram revealed no valvular or wall motion abnormalities. A CT abdomen and pelvis was done given an unclear source of infection in the setting of transaminitis. It revealed multiple hypo-attenuating indeterminate liver lesions. MRI demonstrated liver lesions suspicious for abscesses along with partial middle hepatic vein thrombosis. Blood cultures grew Klebsiella Pneumoniae. The liver abscesses were too small to drain. A PICC line was placed for six weeks of ceftriaxone. For hepatic vein thrombosis treatment the patient was started on Xarelto. Electrophysiology (EP) was consulted and attributed the Brugada pattern to persistent high fever in the setting of severe sepsis. They felt that no intervention was warranted at that time and the patient was monitored on telemetry without any further EKG abnormalities. Two months later the patient was asymptomatic and repeat CT showed complete resolution of liver abscesses.
Discussion: KLA syndrome was initially described in Southeastern Asia, due to the regional prevalence of K1 and K2 capsular subtypes of K. Pneumoniae which confer resistance to macrophage clearance. Newer case reports document increased incidence in other geographical regions. Mortality rates of up 11% have been reported with metastatic infectious spread being the main prognostic indicator. Some of the most worrisome complications include endophthalmitis, meningitis and multiple organ abscess formation. The mainstay treatment includes antibiotics with abscess drainage if possible.
Our patient also presented with a Brugada pattern on initial EKG, however did not meet diagnostic criteria for Brugada Syndrome as outlined in the 2005 Heart Rhythm Society consensus statement. The presence of fever (as seen in our patient) has been well established as pro-arrhythmogenic and is known to induce the Brugada pattern. EP did not deem our patient to be high risk with Brugada Syndrome, which would warrant immediate AICD placement. He was however educated with regards to the importance of tight fever control, avoidance of certain medications and close outpatient EP followup.
Conclusions: KLA syndrome is associated with high morbidity and mortality when not identified and treated in it’s early stages to prevent multiple organ involvement. Urgent abscess drainage and antibiotic treatment is considered a crucial prognostic determinant. With regards to Brugada, patient’s who display this EKG pattern warrant extensive education and immediate evaluation for Brugada Syndrome diagnosis with risk stratification given the fear of sudden cardiac death.