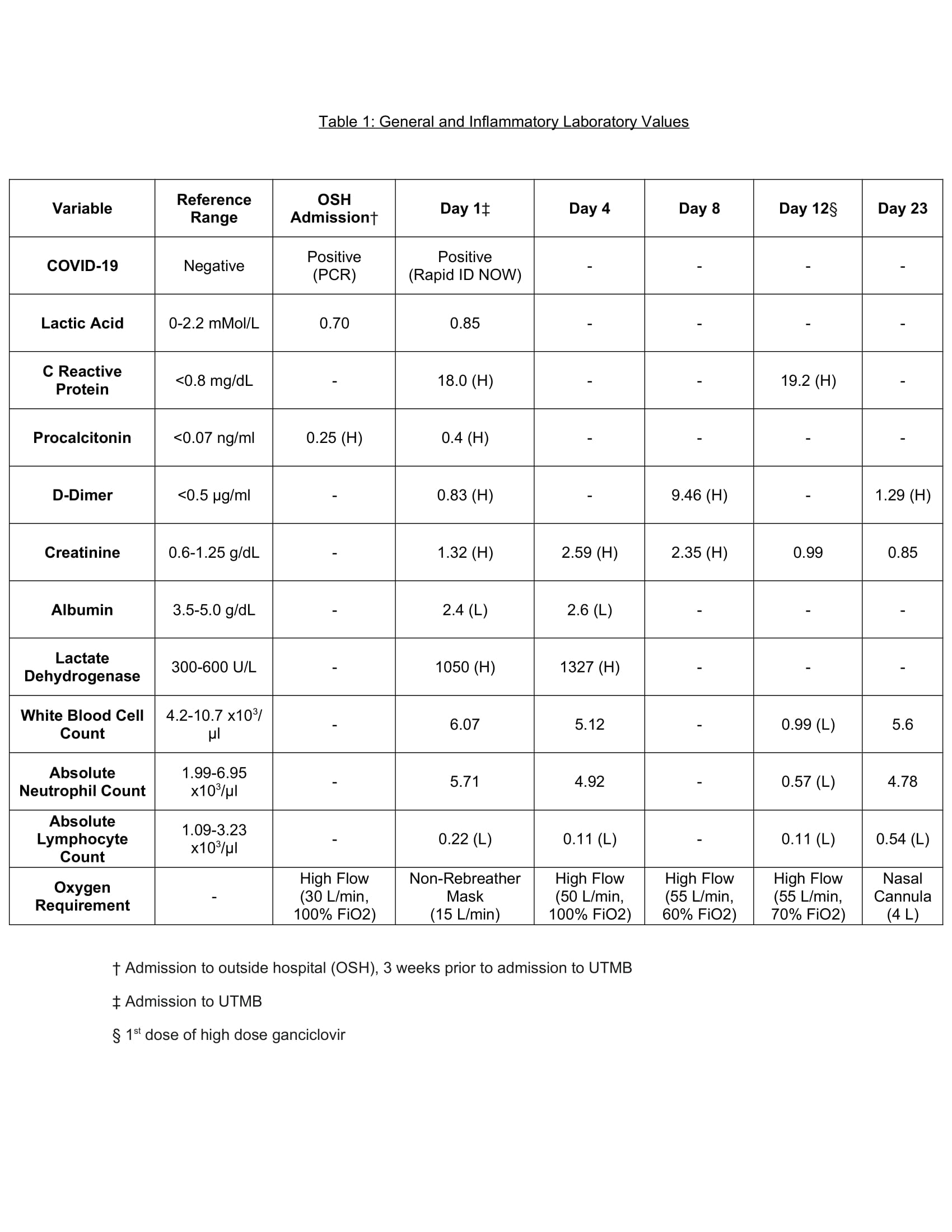
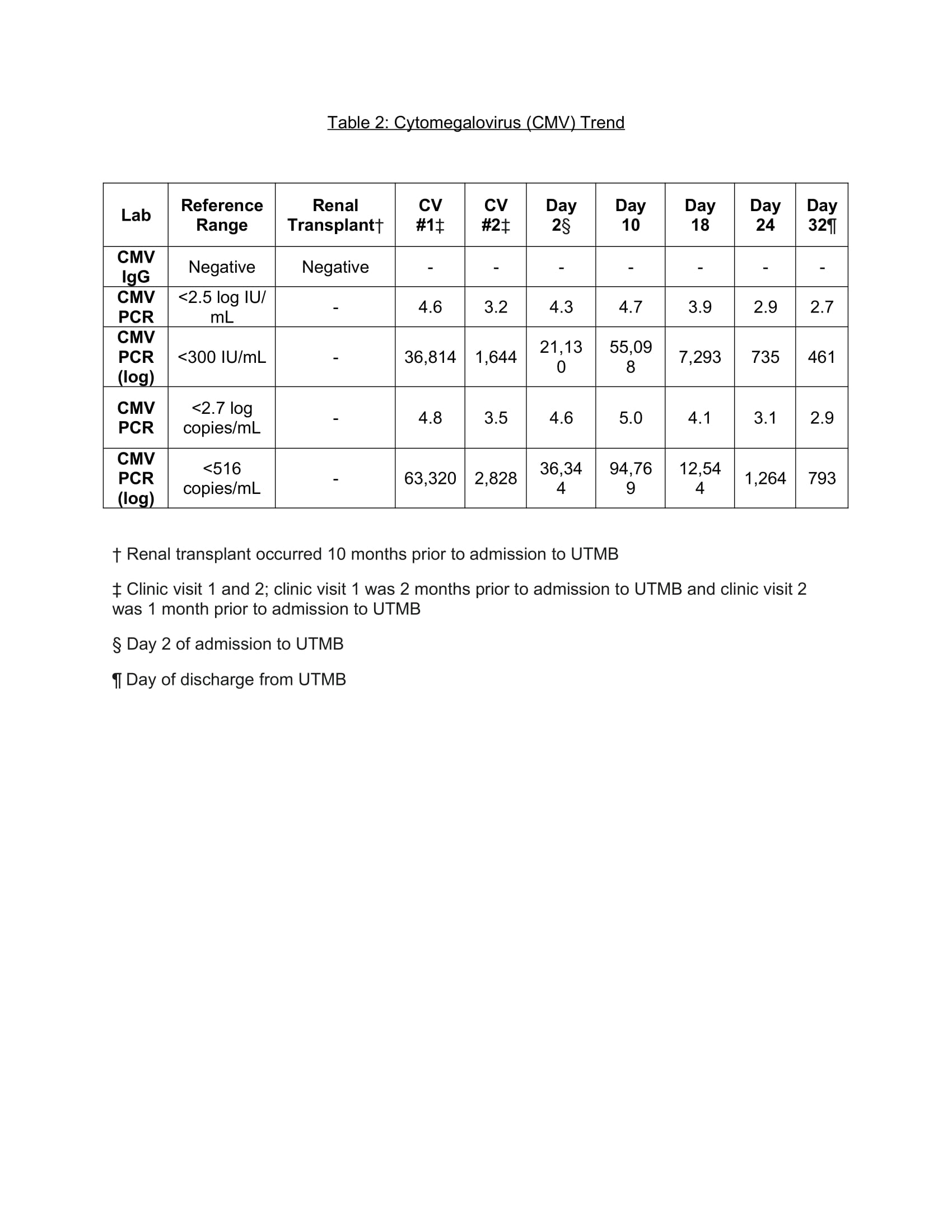
Case Presentation: A 36-year-old male with a renal transplant (CMV serostatus: donor positive/recipient negative) presented to an outside hospital with fever and acute hypoxic respiratory failure requiring high flow oxygen. His maintenance immunosuppressants included cyclosporine and mycophenolate. Upon admission, he was started on treatment for community acquired pneumonia and severe COVID-19 pneumonia. Due to lack of clinical improvement after two weeks, he was started on empiric Pneumocystis Jiroveci (PJP) treatment and his antimicrobial coverage was broadened with no clinical improvement. The patient was then transferred to our hospital three weeks after admission to outside hospital. His CMV viral load was noted to have increased ten-fold in one month while on prophylactic valganciclovir. Given high oxygen requirements, the pulmonary team believed it would not be safe to perform bronchoscopy for biopsy. Given high suspicion of ganciclovir resistant CMV pneumonitis, he was started on high dose ganciclovir with resolution of fever. He was discharged without supplemental oxygen and was switched to Letermovir for CMV prophylaxis.
Discussion: Our patient’s risk factors for developing active CMV disease included being a CMV seronegative recipient of a seropositive donor as well as treatment with over two weeks of dexamethasone for his COVID-19 pneumonia. Moreover, his CMV resistance panel showed a UL97-c603w mutation which should be treated with Foscarnet per guidelines. However, Foscarnet was avoided as the patient clinically improved on high dose ganciclovir. The gold standard for diagnosis of invasive CMV disease is biopsy showing inclusion bodies. While we were unable to obtain a tissue sample, we believe we can support our diagnosis of CMV pneumonia based on decreasing serum CMV viral load in the setting of clinical improvement after treatment with high dose ganciclovir.
Conclusions: Patients with solid organ transplants receiving chronic immunosuppressive therapy are at particular risk for severe disease caused by acquiring a variety of opportunistic pathogens, including cytomegalovirus (CMV). To our knowledge, this is one of the first reports of co-infection of CMV pneumonia and COVID-19 pneumonia.