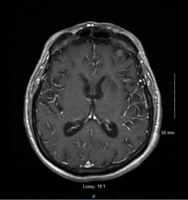
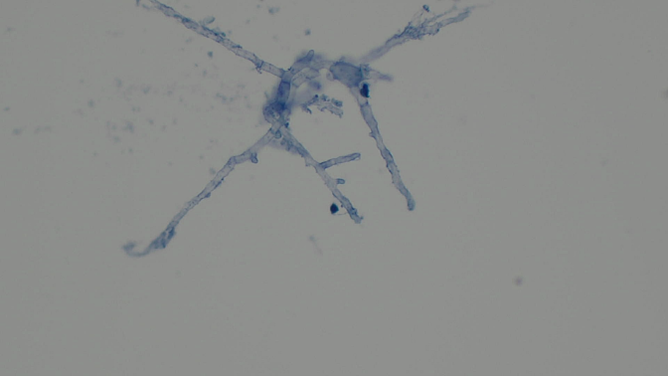
Case Presentation: A 71-year-old male with a history of chronic lymphocytic leukemia (CLL) presented with shortness of breath and weakness. He had been diagnosed with CLL eight years ago and was placed on acalabrutinib 3 months previously. He was hospitalized twice in the prior 2 months for pneumonia.The patient was found to be tachycardic (102/min), hypoxic (91% on 4L nasal cannula), febrile (38.5 °C), and normotensive. Initial work-up was significant for WBC of 8.9 x10 3/mcL. CT Angiography was remarkable for right upper lobe pneumonia with new moderate right pleural effusion and known lymphadenopathy. He was started on vancomycin, azithromycin, and cefepime. Two days later, the patient became acutely hypoxemic and developed cardiac arrest, after which he was intubated. Follow-up chest CT revealed residual mass-like consolidation in the right upper lobe and worsening right pleural effusion, requiring chest tube placement. Sputum culture, bronchoalveolar lavage (BAL), and a CT-guided percutaneous biopsy was obtained from the mass. Brain MRI revealed multiple acute infarcts in the bilateral cerebellar hemispheres, bilateral frontal and parietal lobes, and the left basal ganglia. Mild peripheral enhancement was seen in some infarcts, and repeat MRI revealed interval development of ring enhancement of most lesions (image 1). Antibiotics were changed to meropenem, and liposomal amphotericin B was started. Voriconazole was added following repeat MRI. CSF analysis showed normal WBC, protein, and glucose. CSF galactomannan index was positive (5.79), while CSF fungal cultures were negative.The cytology from the lung biopsy showed septate hyphae suggestive of Aspergillus species (image 2), while the lung tissue showed focal necrosis, fibrosis, and chronic inflammation. The serum galactomannan index was 2.125, serum B-D Glucan was >500 pg/mL, and the BAL galactomannan index was 9.15. BAL mycobacterial smear and Pneumocystis jirovecii PCR were negative. The antibiotics subsequently were narrowed to voriconazole. The sputum and BAL cultures ultimately grew Aspergillus fumigatus. Unfortunately, the patient passed away.
Discussion: Oral bruton tyrosine kinase inhibitors are now standard therapy for relapsed CLL. Invasive fungal infections are a rare but often fatal complication. Acalabrutinib is a recently approved, highly selective BTK inhibitor with the potential to improve tolerability. Despite improved outcomes, cases of invasive fungal infections caused by Aspergillus spp. and Pneumocystis jirovecii have been reported, often occurring within the first few months of therapy. To our knowledge, this is the first reported case of acalabrutinib associated pulmonary and central nervous system aspergillosis with suspected hematogenous dissemination.Our patient progressed despite treatment, in concordance with the high mortality of cerebral aspergillosis of 88%. Early testing of fungal markers can aid in detection and early treatment. Serum galactomannan assay carries a sensitivity and specificity of 0.70 and 0.92 for patients with hematological malignancy and can be detected prior to the development of clinical signs or symptom. CSF galactomannan was utilized in this case which carries a sensitivity of 88.2%.
Conclusions: This case highlights the importance of considering invasive fungal infections in patients recently initiated on acalabrutinib. Fungal markers are a useful, non-invasive tool which can allow for early detection and timely management.