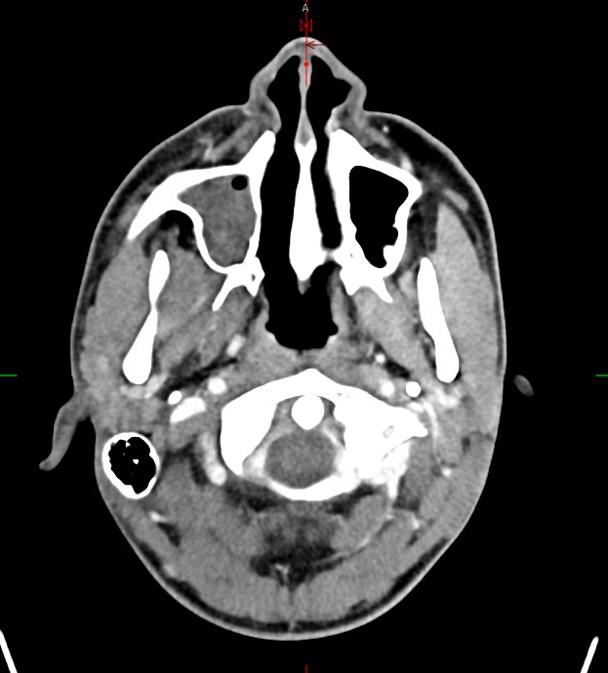
Case Presentation: An 18 year old male presented with ten days of fever, sinus congestion, cough, right sided headache, myalgia and diarrhea. He had no significant past medical history but recently travelled to Bahia, Brazil and engaged in ocean swimming and sushi consumption. He had tested positive for Influenza A at his primary care office five days prior to admission and did not receive treatment. On presentation he was febrile and tachycardic. His physical exam was notable for jaundice, peri-orbital swelling, and mild right upper quadrant tenderness. Laboratory examination revealed leukocytosis, elevated c-reactive protein, hyperbilirubinemia, mild transaminitis, elevated alkaline phosphatase, and negative Influenza. Imaging work up revealed right frontal scalp cellulitis with post septal orbital involvement, sinusitis with subgaleal abscess, and edematous gallbladder. He was started on broad spectrum antibiotics, but continued to have fevers and ultimately underwent lumbar puncture which was unrevealing. Blood cultures on hospital day four speciated penicillin-sensitive Fusobacterium necrophorum. His fever, facial swelling, as well as hyperbilirubinemia resolved over the following days and he was transitioned to amoxicillin and metronidazole on discharge. Internal jugular thrombosis was ruled out.
Discussion: Fusobacterium necrophorum (F. necrophorum) is a non-spore forming gram-negative, anaerobic non-motile bacillus. Compared to other fusobacterium, it has a unique appearance on gram stain with filaments, short rods, and coccoid elements. F. necrophorum can take up to five days to grow in culture. It is primarily found as a part of the normal human flora within the mouth, upper respiratory tract, GI tract, and female genitourinary tract. First reports of human systemic infection with F. necrophorum were identified by Veillon and Zuber in 1898 in a child with chronic purulent otitis media, septic arthritis of the knee, cerebral abscess, and signs of systemic infection. Severe infections typically affect young, otherwise healthy adults. Fusobacterium necrophorum is most commonly known as the cause of postanginal sepsis with suppurative thrombophlebitis of the jugular vein, otherwise known as Lemierre’s syndrome. The lesser known otogenic variant can also cause dental abscesses, peritonsillar abscesses, pharyngotonsillitis, mastoiditis and even intracranial complications such as meningitis and sinus thrombosis. This patient developed a post-influenza, non-Lemierre syndrome Fusobacterium infection with sinusitis, facial cellulitis, and jaundice. Post-influenza Fusobacterium infection has been rarely reported in the literature.
Conclusions: Fusobacterium necrophorum is a gram negative bacteria most commonly found in normal oropharyngeal flora. Infectious symptoms can initially be misdiagnosed for other oropharyngeal infections, such as streptococcus pyogenes. F. necrophorum can lead to serious infections and there are no PCR or rapid test available. This case demonstrates the need to consider F. necrophorum etiology in a young patient with worsening systemic symptoms after an Influenza diagnosis.