Background: Intensive Care Unit (ICU) beds are limited, so effective triage is important for resource utilization. However, inappropriate triage of critically ill patients to non ICU settings can lead to poor patient outcomes, as early unexpected ICU transfers are associated with increased mortality.
Purpose: We sought to describe the effectiveness of Hospital Medicine (HM), Emergency Medicine (EM) and Critical Care (CC) collaboration in triaging critically ill patients as well as understand where opportunities lie for improvement.
Description: Data was collected from the EMR of a 900 bed, academic urban safety net hospital, on all patients admitted to the MICU or admitted to the medical ward and transferred to the ICU within 24hrs over four weeks starting September 15, 2017. Cases were classified as potential False Positive ICU admissions if admitted to ICU and transferred to the floor or discharged within 24 hours. Potential False Negatives were defined as patients who were either discharged from the ED and admitted to the ICU within 24 hours or admitted to a ward team and transferred to the ICU within 24 hours. Potential False Positives and False Negatives were reviewed by ICU faculty to determine the appropriateness of initial triage. Multidisciplinary meetings with CC, HM and EM faculty were held to discuss all cases of suspected inappropriate triage.
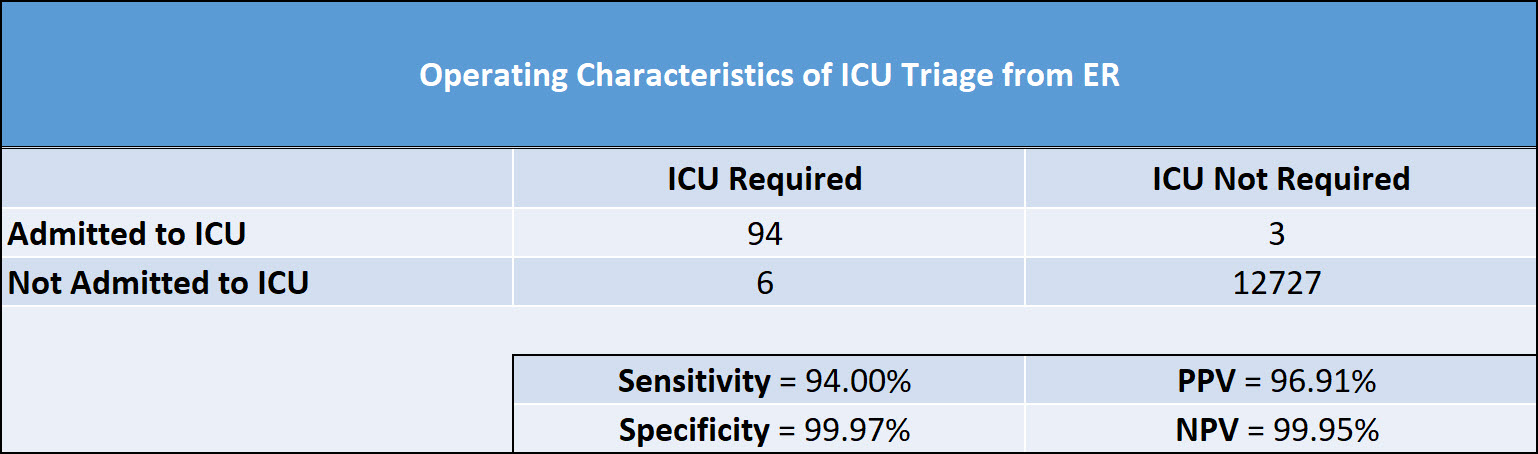
Conclusions: During this 4 week period in September 2017, 97 patients of 12,830 total patients (0.76%) triaged in the ED were admitted to the MICU. After review, only 3 of the total 19 potential false positives were deemed unnecessary ICU admissions. The diagnoses included one end stage ILD patient, one patient with concern for serotonin syndrome, and one patient with asthma on continuous nebulizers. Of the 10 potential false negative patients, 6 patients were deemed to be inappropriately triaged to a ward team on presentation. See Figure for sensitivity, specificity and positive and negative predictive values.
Review of our data shows very high specificity (99.97%) with 84.2% of 24 hour admissions to the MICU deemed necessary, suggesting that our system of collaborative triage between EM, CC and HM is very effective in MICU resource utilization. Sensitivity is also high (94%) but may have room for improvement. With 1.5 false negatives a week, decreasing the false negative rate by 66% to 0.5 per week would result in a sensitivity of 98%. Implementing predictive analytics in the ED to detect patients at high risk of clinical deterioration may allow us to increase sensitivity without adversely affecting specificity.
There are no current guidelines to inform how well our system performs compared to norms. Working with other health systems to establish operational norms could improve overall efficiency and safety of ICU triage from the ED.
.jpg)
