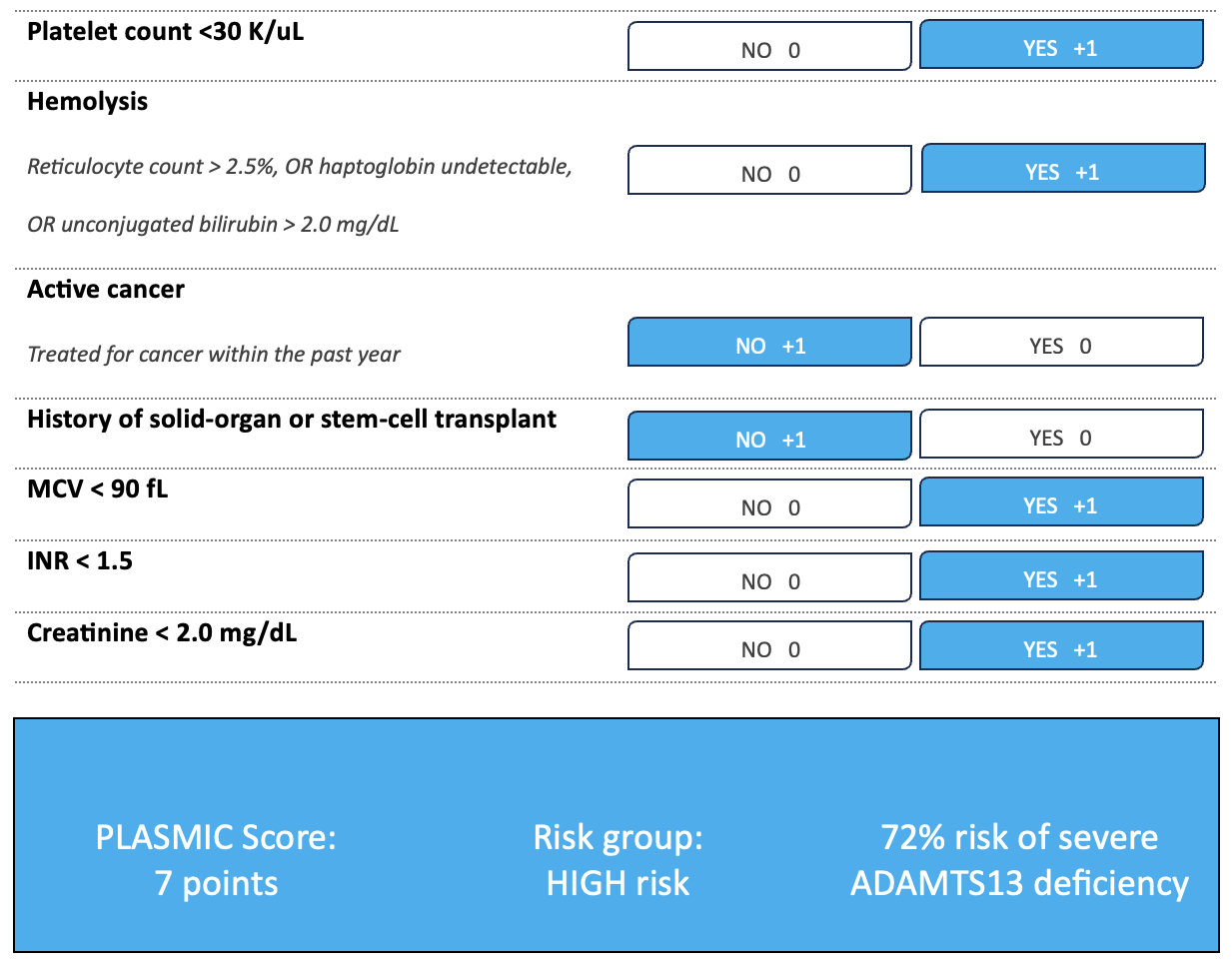
Case Presentation: A 29-year-old female Jehovah’s Witness presented with three weeks of easy bruising in the absence of trauma. She also noticed heavier and prolonged menstrual flow associated with fatigue and dizziness. She denied medication use, febrile illnesses or neurologic symptoms. Vital signs were normal. Physical exam revealed multiple ecchymoses on bilateral upper and lower extremities. There was no scleral icterus, lymphadenopathy or splenomegaly. Lab investigations were significant for normocytic anemia, thrombocytopenia, elevated lactate dehydrogenase, undetectable haptoglobin, unconjugated hyperbilirubinemia, schistocytes on blood film and undetectable ADAMTS13 with increased inhibitor activity, thus diagnosing acquired thrombotic thrombocytopenic purpura (aTTP) (Figure 1 & Table 1). The patient was started on high-dose corticosteroids and caplacizumab. With respect to her religious beliefs, transfusion of fresh frozen plasma (FFP) was not an option for therapeutic plasma exchange (TPE). However, she was willing to accept minor fractions of blood that were permissible by her faith, including plasma derivatives, such as cryosupernatant plasma (CSP) and albumin. Due to severe hypersensitivity to CSP, she completed a total of eight daily plasma exchanges using three liters of 5% human albumin solution as the replacement fluid. She also accepted human fibrinogen concentrate to correct the resulting hypofibrinogenemia. Clinical improvement was observed with TPE. The platelet count stabilized above 150K/uL starting on day six and no new areas of bruising or bleeding were noted. The anemia reached a nadir of 7.0 g/dL but improved with hematinics and treatment of the aTTP. She was discharged on medical therapy to follow up with hematology. Serial labs showed incremental normalization of all hematological derangements and ongoing surveillance over one year showed no relapse.
Discussion: aTTP is a rare hematologic emergency caused by an autoimmune deficiency of ADAMTS13, a von Willebrand factor (vWF) cleaving protease, leading to microthrombi formation, ischemia and end organ dysfunction [1,2]. In 20-30% of cases, aTTP involves a pentad: fever, microangiopathic hemolytic anemia, thrombocytopenia, renal failure and neurologic dysfunction [1,2]. Daily TPE using FFP or CSP forms first-line treatment to replete ADAMTS13 and remove its autoantibodies. CSP is beneficial due to relative deficiency of vWF multimers, which are implicated in the pathogenesis of aTTP. If not treated, mortality from TTP is 90% [2]. In view of religious contraindication to FFP and CSP hypersensitivity, 5% human albumin solution was successfully used as the sole plasma exchange fluid to initiate clinical remission of aTTP in our patient, alongside caplacizumab and immunosuppressive therapy. Similar outcomes were observed in five reported episodes of aTTP in Jehovah’s Witnesses, redemonstrating that successful TPE is possible with human albumin solution [3]. This novel and patient-centered approach in our bloodless patient emphasizes the high-quality outcomes possible with the transfusion-restrictive strategies of patient blood management [4].
Conclusions: Human albumin solution was a safe alternative plasma exchange fluid for induction of clinical remission of aTTP in a bloodless patient, with adjunct medical therapies. This may help solve ethical challenges faced in treatment of aTTP when religious beliefs, patient refusal, medical contraindications or product shortages preclude use of FFP or CSP.