Background: Conversations around advance care planning (ACP) allow patients to direct the type and intensity of the medical care that they receive. Known ethnic and racial disparities in ACP exist, with racial and ethnic minorities less likely to have living wills and DNR orders. We aimed to understand the impact of an intervention to improve the documentation of ACP conversations for hospitalized patients on health disparities at our institution.
Methods: In February 2019 the Division of Hospital Medicine at an urban, academic health system launched an initiative to improve rates of documented ACP conversations using new tools available in the electronic medical record (EMR). Hospitalists and trainees were encouraged to document ACP conversations for all patients >75 or with advanced illness as measured by recognized ICD-10 codes. EMR-generated reports provided patient-level compliance and demographics for 5563 discharged or deceased patients who met criteria from July 2018 to October 2019 prior to and following the intervention. ACP completion by discharge was analyzed by self-reported race, ethnicity, and preferred language. Patients with Hispanic or Latino ethnicity were classified as Hispanic/Latino; patients with non-Hispanic or Latino ethnicity were classified by race (White/Caucasian, Black/African-American, Asian, or Other). Self-reported languages were classified as English, Chinese, Russian, Spanish, or Other. Patients with unknown/declined race or language were excluded. We used ANOVA analyses to determine baseline differences and chi square to test the association of the intervention on ACP documentation in racial/ethnic and language groups.
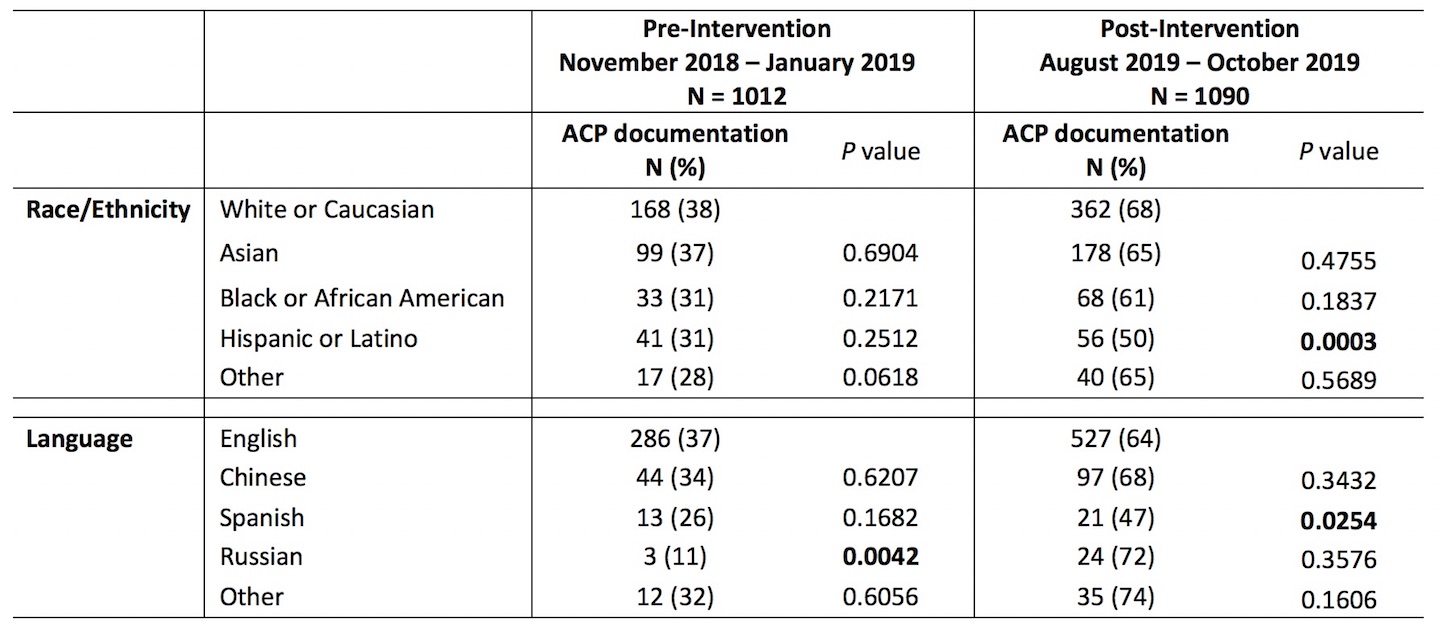
Results: Using the quarter prior to the intervention as a baseline, overall rates of ACP documentation improved significantly when compared to the most recent 3 months of the intervention (356/1012 [35.4%] Nov 2018 – Jan 2019 compared to 740/1090 [64.6%] Aug – Oct 2019, P<0.001). At baseline there were no disparities by race/ethnicity (P=0.182) but significant disparities were associated with patient preferred language (P=0.035), with Russian speaking patients less likely to have ACP documentation compared to English speaking patients (P=0.0042). In the most recent 3 months of the intervention, race/ethnicity (P=0.035) and language (P=0.036) were associated with significant differences in ACP documentation. Using White/Caucasian race as a reference, patients identifying as Hispanic/Latino were significantly less likely to have ACP documentation (P=0.0003). Using English language as a reference, Spanish speaking patients were significantly less likely to have ACP documentation (P=0.0254); there was no longer a difference in ACP documentation rates for Russian speaking patients (Table).
Conclusions: An intervention designed to improve ACP documentation resulted in overall improved rates of documented ACP conversations for hospitalized medical patients. However, the intervention was associated with new disparities for Hispanic/Latino and Spanish speaking patients. Further analyses are needed to explore the interaction between ethnic and language disparities and the underlying patient, provider, and system-level factors associated with these identified disparities.